Association of dementia with impaired kidney function and plasma biomarkers: A population-based study
Abstract
Background and Purpose
Emerging evidence has linked impaired kidney function with dementia in older adults, but the neuropathological pathways underlying their association remain poorly understood. We sought to examine the relationships of kidney function with dementia and plasma biomarkers in a Chinese rural population.
Methods
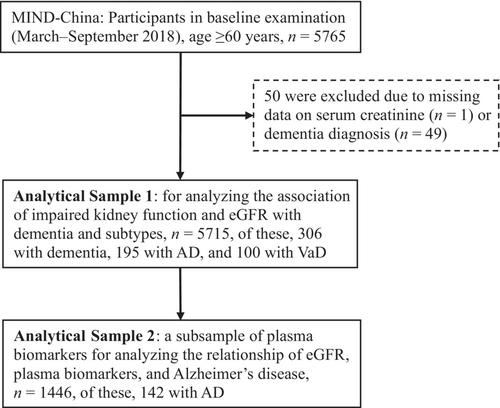
This population-based study used data from the baseline examination of the Multimodal Interventions to Delay Dementia and Disability in rural China (MIND-China) cohort (March–September 2018; n = 5715). Kidney function was assessed using estimated glomerular filtration rate (eGFR) based on serum creatinine level. Dementia, Alzheimer's disease (AD) and vascular dementia (VaD) were diagnosed according to the international criteria. Plasma biomarkers were measured using the SIMOA platform in a subsample (n = 1446). Data were analyzed using logistic, general linear, and mediation models.
Results
Of the 5715 participants, 306 were diagnosed with dementia, including 195 with AD and 100 with VaD. Impaired kidney function (eGFR <60 vs. ≥90 mL/min/1.73 m2) was associated with multivariable-adjusted odds ratios of 2.24 (95% confidence interval [CI] 1.44–3.46) for all-cause dementia, 1.85 (1.07–3.18) for AD, and 2.49 (1.16–5.22) for VaD. In the biomarker subsample, impaired kidney function was significantly associated with higher plasma amyloid-β (Aβ)40 (β-coefficient = 54.36, 95% CI 43.34–65.39), Aβ42 (β-coefficient = 3.14, 95% CI 2.42–3.86), neurofilament light chain (β-coefficient = 10.62, 95% CI 5.62–15.62), and total tau (β-coefficient = 0.68, 95% CI 0.44–0.91), and a lower Aβ42/Aβ40 ratio (β-coefficient = −4.11, 95% CI −8.08 to −0.14). The mediation analysis showed that plasma total tau significantly mediated 21.76% of the association between impaired kidney function and AD (p < 0.05).
Conclusion
Impaired kidney function is associated with dementia and plasma biomarkers among rural-dwelling older Chinese adults, and the association with AD is partly mediated by plasma biomarkers for neurodegeneration.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


