Prognostic role of pre-diagnostic circulating inflammatory biomarkers in breast cancer survival: evidence from the EPIC cohort study
IF 6.4
1区 医学
Q1 ONCOLOGY
引用次数: 0
Abstract
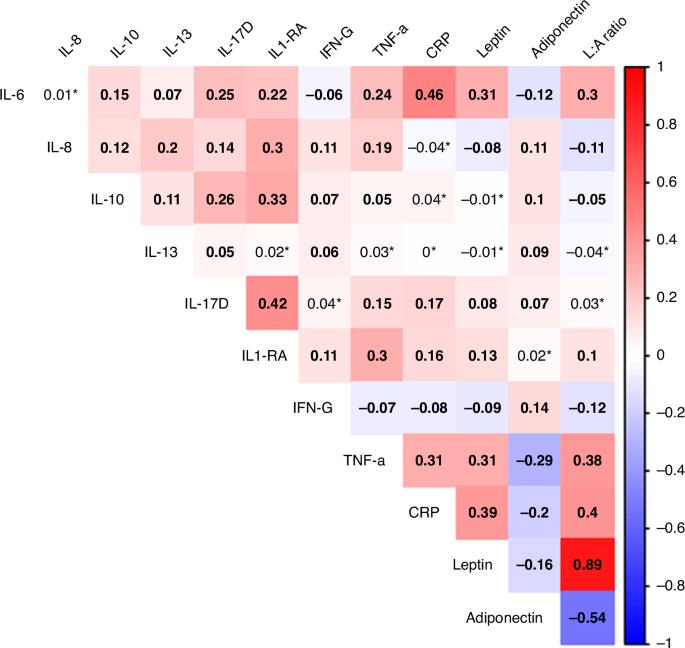
Inflammation influences tumour progression and cancer prognosis, but its role preceding breast cancer (BC) and its prognostic implications remain inconclusive. We studied pre-diagnostic plasma inflammatory biomarkers in 1538 women with BC from the EPIC study. Cox proportional hazards models assessed their relationship with all-cause and BC-specific mortality, adjusting for tumour characteristics and lifestyle factors. Over a 7-year follow-up after diagnosis, 229 women died, 163 from BC. Elevated IL-6 levels were associated with increased all-cause mortality risk (HR1-SD 1.25, 95% CI 1.07–1.47). Among postmenopausal, IL-6 was associated with higher all-cause (HR1-SD 1.41, 95% CI 1.18–1.69) and BC-specific mortality (HR1-SD 1.31, 95% CI 1.03–1.66), (PHeterogeneity (pre/postmenopausal) < 0.05 for both), while IL-10 and TNFα were associated with all-cause mortality only (HR1-SD 1.19, 95% CI 1.02–1.40 and HR1-SD 1.28, 95% CI 1.06–1.56). Among ER+PR+, IL-10 was associated with all-cause and BC-specific mortality (HR1-SD 1.35, 95% CI 1.10–1.65 and HR1-SD 1.42 95% CI 1.08–1.86), while TNF-α was associated with all-cause mortality in HER2- (HR1-SD 1.31, 95% CI 1.07–1.61). An inflammatory score predicted higher all-cause mortality, especially in postmenopausal women (HR1-SD 1.30, 95% CI 1.07–1.58). Higher pre-diagnosis IL-6 levels suggest poorer long-term survival among BC survivors. In postmenopausal survivors, elevated IL-6, IL-10, and TNFα and inflammatory scores seem to predict all-cause mortality.
诊断前循环炎症生物标志物在乳腺癌生存中的预后作用:来自 EPIC 队列研究的证据。
背景:炎症影响肿瘤的进展和癌症的预后,但其在乳腺癌(BC)前的作用及其预后意义仍无定论:我们研究了EPIC研究中1538名乳腺癌女性患者的诊断前血浆炎症生物标志物。Cox比例危险模型评估了它们与全因死亡率和BC特异性死亡率的关系,并对肿瘤特征和生活方式因素进行了调整:结果:在确诊后的7年随访中,229名女性死亡,其中163人死于BC。IL-6水平升高与全因死亡风险增加有关(HR1-SD 1.25,95% CI 1.07-1.47)。在绝经后人群中,IL-6与更高的全因死亡率(HR1-SD 1.41,95% CI 1.18-1.69)和BC特异性死亡率(HR1-SD 1.31,95% CI 1.03-1.66)相关(异质性(绝经前/绝经后)1-SD 1.19,95% CI 1.02-1.40和HR1-SD 1.28,95% CI 1.06-1.56)。在 ER+PR+ 中,IL-10 与全因死亡率和 BC 特异性死亡率相关(HR1-SD 1.35,95% CI 1.10-1.65 和 HR1-SD 1.42,95% CI 1.08-1.86),而 TNF-α 与 HER2- 的全因死亡率相关(HR1-SD 1.31,95% CI 1.07-1.61)。炎症评分预示着较高的全因死亡率,尤其是绝经后妇女(HR1-SD 1.30,95% CI 1.07-1.58):结论:诊断前IL-6水平越高,表明乳腺癌幸存者的长期生存率越低。在绝经后幸存者中,IL-6、IL-10、TNFα和炎症评分的升高似乎可预测全因死亡率。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
British Journal of Cancer
医学-肿瘤学
CiteScore
15.10
自引率
1.10%
发文量
383
审稿时长
6 months
期刊介绍:
The British Journal of Cancer is one of the most-cited general cancer journals, publishing significant advances in translational and clinical cancer research.It also publishes high-quality reviews and thought-provoking comment on all aspects of cancer prevention,diagnosis and treatment.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


