Recommendations from the 2024 Australian evidence-based guideline for unexplained infertility: ADAPTE process from the ESHRE evidence-based guideline on unexplained infertility
Abstract
Introduction
The 2024 Australian evidence-based guideline for unexplained infertility provides clinicians with evidence-based recommendations for the optimal diagnostic workup for infertile couples to establish the diagnosis of unexplained infertility and optimal therapeutic approach to treat couples diagnosed with unexplained infertility in the Australian health care setting. The guideline recommendations were adapted for the Australian context from the rigorous, comprehensive European Society of Human Reproduction and Embryology (ESHRE) 2023 Evidence-based guideline: unexplained infertility, using the ADAPTE process and have been approved by the Australian National Health and Medical Research Council.
Main recommendations
- definition — defining infertility and frequency of intercourse, infertility and age, female and male factor infertility;
- diagnosis — ovulation, ovarian reserve, tubal factor, uterine factor, laparoscopy, cervical/vaginal factor, male factor, additional testing for systemic conditions; and
- treatment — expectant management, active treatment, mechanical-surgical procedures, alternative therapeutic approaches, quality of life.
Changes in assessment and management resulting from the guideline
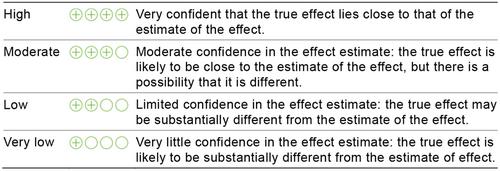
This guideline refines the definition of unexplained infertility and addresses basic diagnostic procedures for infertility assessment not considered in previous guidelines on unexplained infertility. For therapeutic approaches, consideration of evidence quality, efficacy, safety and, in the Australian setting, feasibility, acceptability, cost, implementation and ultimately recommendation strength were integrated across multidisciplinary expertise and consumer perspectives in adapting recommendations to the Australian context by using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) framework, which had not been used in past guidelines on unexplained infertility to formulate recommendations. The Australian process also included an established data integrity check to ensure evidence could be trusted to guide practice. Practice points were added and expanded to consider the Australian setting. No evidence-based recommendations were underpinned by high quality evidence, with most having low or very low quality evidence. In this context, research recommendations were made including those for the Australian context. The full guideline and technical report are publicly available online and can be accessed at https://www.monash.edu/medicine/mchri/infertility and are supported by extensive translation resources, including the free patient ASKFertility mobile application (https://www.askfertility.org/).

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


