Multicenter, open label, randomized controlled superiority trial for availability to reduce nocturnal urination frequency: The TOP-STAR study
Abstract
Aim
Nocturia impairs the quality of life in patients with type 2 diabetes mellitus. Although sodium glucose co-transporter 2 inhibitors (SGLT2i) such as tofogliflozin increase urine volume, their impact on nocturia, in conjunction with dietary salt restriction, is less clear.
Materials and Methods
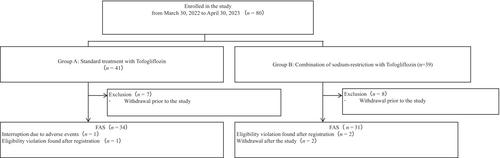
This multicenter, open-label, randomized, parallel-group trial included 80 subjects with type 2 diabetes and nocturia. The patients were divided into two groups: one receiving tofogliflozin, the shortest half-life, without salt restriction, and the other receiving both tofogliflozin and dietary salt restriction. The primary endpoint was nocturia frequency at 12 weeks. The secondary outcomes included changes in daytime urination frequency, urine volume, and home blood pressure.
Results
At 12 weeks, there were no significant differences in nocturia changes between both groups. Nocturia frequency did not change in the tofogliflozin without salt restriction group from 1.5 ± 0.8 to 1.3 ± 1.1 times per night (P = 0.297), and significantly decreased from 1.6 ± 1.0 to 1.3 ± 0.7 times per night in the tofogliflozin and dietary salt restriction group (P = 0.049). There was a trend toward increased urine volume and frequency during the daytime in the group with salt restriction, indicating a time-shift effect of the short half-life tofogliflozin and salt restriction on urinary time.
Conclusions
The frequency of nocturia after tofogliflozin did not increase. Tofogliflozin reduced nocturia when combined with salt restriction. Furthermore, daytime urine volume and frequency showed an increasing trend, suggesting a shift in urine production to daytime hours due to the short half-life of tofogliflozin. Dietary modifications can enhance the therapeutic benefits of tofogliflozin in managing nocturia in people with type 2 diabetes.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


