A randomized trial testing digital medicine support models for mild-to-moderate alcohol use disorder
IF 12.4
1区 医学
Q1 HEALTH CARE SCIENCES & SERVICES
引用次数: 0
Abstract
This paper reports the results of a hybrid effectiveness-implementation randomized trial that systematically varied levels of human oversight required to support the implementation of a digital medicine intervention for persons with mild-to-moderate alcohol use disorder (AUD). Participants were randomly assigned to three groups representing possible digital health support models within a health system: self-monitored use (SM; n = 185), peer-supported use (PS; n = 186), or a clinically integrated model CI; (n = 187). Across all three groups, the percentage of self-reported heavy drinking days dropped from 38.4% at baseline (95% CI [35.8%, 41%]) to 22.5% (19.5%, 25.5%) at 12 months. The clinically integrated group showed significant improvements in mental health and quality of life compared to the self-monitoring group (p = 0.011). However, higher attrition rates in the clinically integrated group warrant consideration in interpreting this result. Results suggest that making a self-guided digital intervention available to patients may be a viable option for health systems looking to promote alcohol risk reduction. This study was prospectively registered at clinicaltrials.gov on 7/03/2019 (NCT04011644).
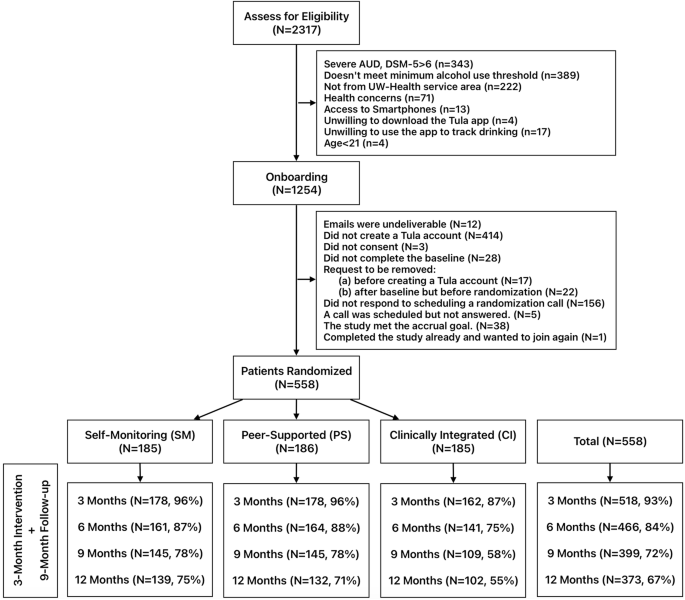
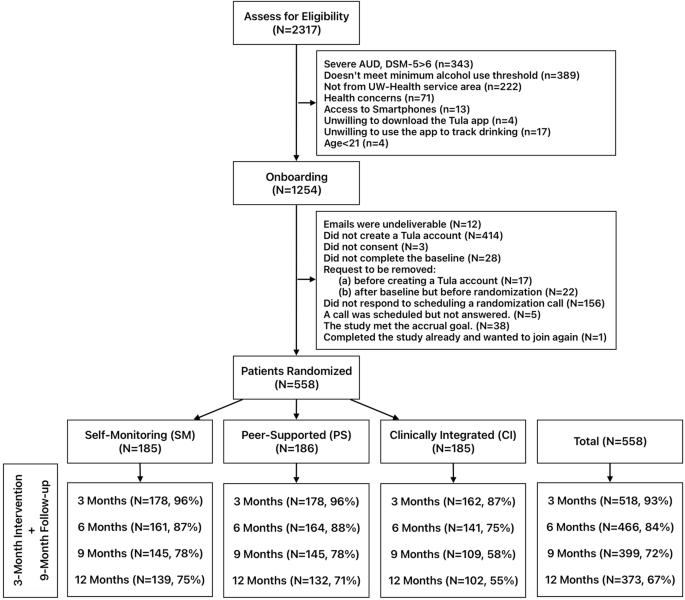
测试轻度至中度酒精使用障碍数字医学支持模式的随机试验
本文报告了一项混合效果-实施随机试验的结果,该试验系统地改变了对轻度至中度酒精使用障碍(AUD)患者实施数字医疗干预所需的人工监督水平。参与者被随机分配到代表医疗系统内可能的数字医疗支持模式的三组:自我监控使用(SM;n = 185)、同伴支持使用(PS;n = 186)或临床整合模式 CI;(n = 187)。在所有三组中,自我报告的大量饮酒天数比例从基线时的 38.4%(95% CI [35.8%,41%])下降到 12 个月时的 22.5%(19.5%,25.5%)。与自我监控组相比,临床综合组在心理健康和生活质量方面有显著改善(p = 0.011)。然而,临床综合组的自然减员率较高,在解释这一结果时应加以考虑。研究结果表明,对于希望促进降低酒精风险的医疗系统来说,向患者提供自我指导的数字干预可能是一个可行的选择。本研究于2019年3月7日在clinicaltrials.gov进行了前瞻性注册(NCT04011644)。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

NPJ Digital Medicine
Multiple-
CiteScore
25.10
自引率
3.30%
发文量
170
审稿时长
15 weeks
期刊介绍:
npj Digital Medicine is an online open-access journal that focuses on publishing peer-reviewed research in the field of digital medicine. The journal covers various aspects of digital medicine, including the application and implementation of digital and mobile technologies in clinical settings, virtual healthcare, and the use of artificial intelligence and informatics.
The primary goal of the journal is to support innovation and the advancement of healthcare through the integration of new digital and mobile technologies. When determining if a manuscript is suitable for publication, the journal considers four important criteria: novelty, clinical relevance, scientific rigor, and digital innovation.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


