Determinants of survival after first relapse of acute lymphoblastic leukemia: a Children’s Oncology Group study
IF 12.8
1区 医学
Q1 HEMATOLOGY
引用次数: 0
Abstract
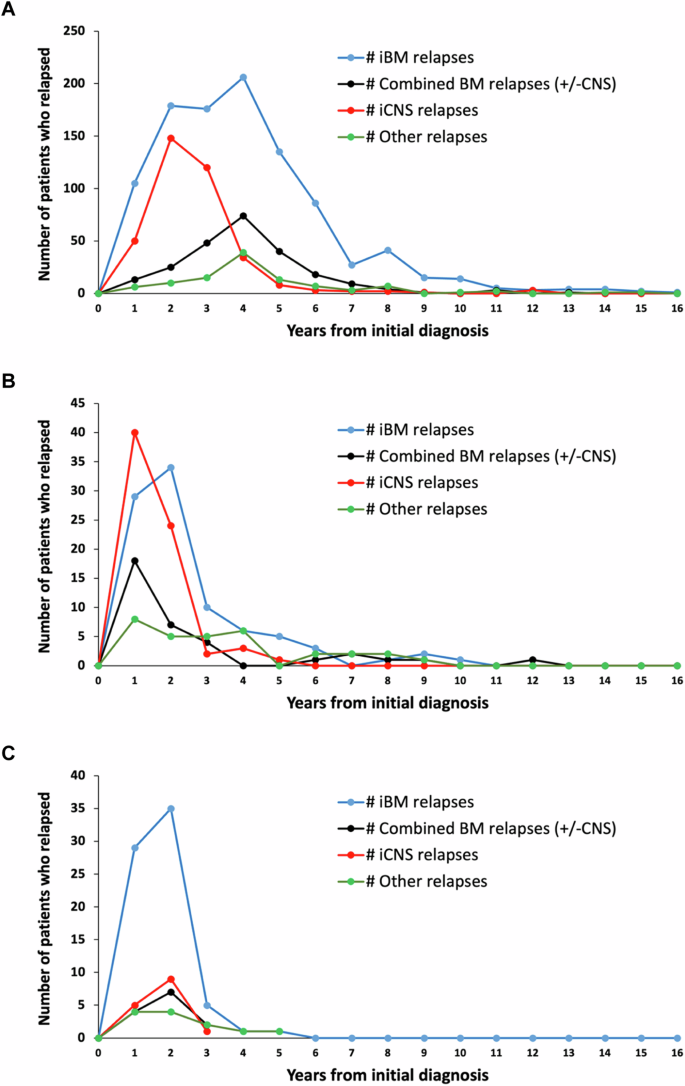
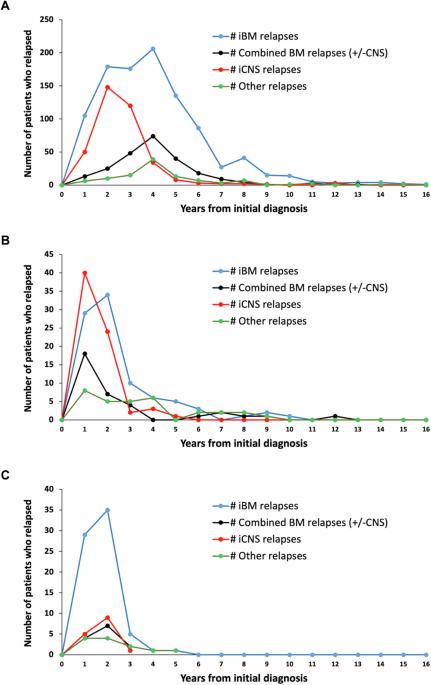
Limited prognostic factors have been associated with overall survival (OS) post-relapse in childhood Acute Lymphoblastic Leukemia (ALL). Patients enrolled on 12 Children’s Oncology Group frontline ALL trials (1996–2014) were analyzed to assess for additional prognostic factors associated with OS post-relapse. Among 16,115 patients, 2053 (12.7%) relapsed. Relapse rates were similar for B-ALL (12.5%) and T-ALL (11.2%) while higher for infants (34.2%). Approximately 50% of B-ALL relapses occurred late (≥36 months) and 72.5% involved the marrow. Conversely, 64.8% of T-ALL relapses occurred early (<18 months) and 47.1% involved the central nervous system. The 5-year OS post-relapse for the entire cohort was 48.9 ± 1.2%; B-ALL:52.5 ± 1.3%, T-ALL:35.5 ± 3.3%, and infant ALL:21.5 ± 3.9%. OS varied by early, intermediate and late time-to-relapse; 25.8 ± 2.4%, 49.5 ± 2.2%, and 66.4 ± 1.8% respectively for B-ALL and 29.8 ± 3.9%, 33.3 ± 7.6%, 58 ± 9.8% for T-ALL. Patients with ETV6::RUNX1 or Trisomy 4 + 10 had median time-to-relapse of 43 months and higher OS post-relapse 74.4 ± 3.1% and 70.2 ± 3.6%, respectively. Patients with hypodiploidy, KMT2A-rearrangement, and TCF3::PBX1 had short median time-to-relapse (12.5-18 months) and poor OS post-relapse (14.2 ± 6.1%, 31.9 ± 7.7%, 36.8 ± 6.6%). Site-of-relapse varied by cytogenetic subtype. This large dataset provided the opportunity to identify risk factors for OS post-relapse to inform trial design and highlight populations with dismal outcomes post-relapse.
急性淋巴细胞白血病首次复发后存活的决定因素:儿童肿瘤学小组的一项研究
与儿童急性淋巴细胞白血病(ALL)复发后总生存期(OS)相关的预后因素有限。我们分析了12项儿童肿瘤学组一线ALL试验(1996-2014年)的入组患者,以评估与复发后OS相关的其他预后因素。在16115名患者中,有2053人(12.7%)复发。B-ALL(12.5%)和T-ALL(11.2%)的复发率相似,而婴儿的复发率更高(34.2%)。约50%的B-ALL复发发生在晚期(≥36个月),72.5%的复发涉及骨髓。相反,64.8%的T-ALL复发发生在早期(18个月),47.1%累及中枢神经系统。整个队列的复发后5年OS为(48.9 ± 1.2%);B-ALL为(52.5 ± 1.3%),T-ALL为(35.5 ± 3.3%),婴儿ALL为(21.5 ± 3.9%)。OS因早期、中期和晚期复发时间而异;B-ALL分别为25.8±2.4%、49.5±2.2%和66.4±1.8%,T-ALL分别为29.8±3.9%、33.3±7.6%和58±9.8%。ETV6::RUNX1或4+10三体综合征患者的中位复发时间为43个月,复发后的OS分别为(74.4±3.1)%和(70.2±3.6)%。低二倍体、KMT2A重排和TCF3::PBX1患者的中位复发时间较短(12.5-18个月),复发后的OS较差(14.2±6.1%、31.9±7.7%、36.8±6.6%)。复发部位因细胞遗传亚型而异。这一大型数据集为确定复发后OS的风险因素提供了机会,从而为试验设计提供依据,并突出了复发后结果不佳的人群。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Leukemia
医学-血液学
CiteScore
18.10
自引率
3.50%
发文量
270
审稿时长
3-6 weeks
期刊介绍:
Title: Leukemia
Journal Overview:
Publishes high-quality, peer-reviewed research
Covers all aspects of research and treatment of leukemia and allied diseases
Includes studies of normal hemopoiesis due to comparative relevance
Topics of Interest:
Oncogenes
Growth factors
Stem cells
Leukemia genomics
Cell cycle
Signal transduction
Molecular targets for therapy
And more
Content Types:
Original research articles
Reviews
Letters
Correspondence
Comments elaborating on significant advances and covering topical issues
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


