Are measurable residual disease results after consolidation therapy useful in children with acute lymphoblastic leukemia?
IF 12.8
1区 医学
Q1 HEMATOLOGY
引用次数: 0
Abstract
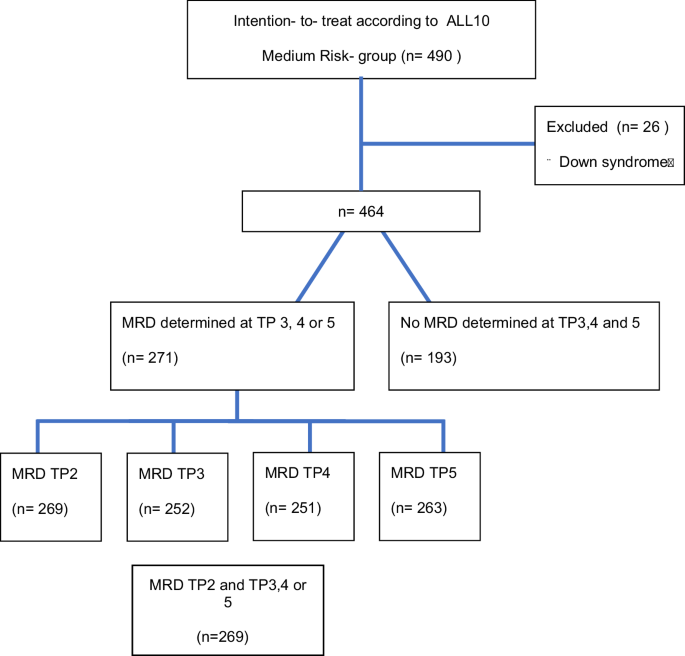
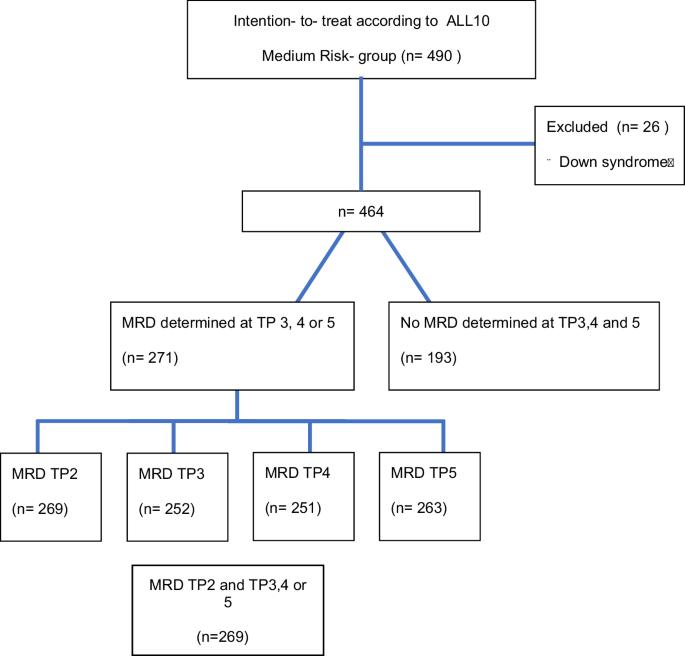
Measurable residual disease (MRD) is regularly tested at later timepoints after the end of first consolidation (EOC) in children with acute lymphoblastic leukemia (ALL). The question remains whether this is useful for detecting (molecular) relapse. We investigated the clinical relevance of MRD after EOC in intermediate risk patients treated on DCOG-ALL-10 (n = 271) and DCOG-ALL-9 (n = 122), with MRD <0.05% at EOC. EOC MRD-negative patients (n = 178) had excellent outcomes, irrespective of MRD results at later timepoints; 6-year cumulative incidence of relapse (6-y CIR) of 7.4% (95% CI, 3.9%–12.3%) for those with MRD negativity at all later timepoints compared to 3.8% (95% CI, 0.3%–16.8%) for those with one or more later timepoints being positive (p = 0.51). Patients with positive EOC MRD (n = 91) of whom the subsequent timepoints were MRD negative (n = 43), had comparable good outcomes, 6-y CIR of 7.0% (95% CI, 1.8%–17.2%). In contrast, patients being MRD positive at EOC and MRD positive at one or more subsequent timepoints (n = 48) had a higher risk of relapse, 6-y CIR 29.4% (95% CI, 17.2%–42.8%), p < 0.001. These findings were confirmed in the validation cohort of ALL-9 as well as using the updated EuroMRD guidelines. In EOC MRD-negative patients, subsequent MRD measurements can be abandoned. For EOC MRD-positive patients the subsequent MRD measurement might be informative for further risk stratification.
急性淋巴细胞白血病患儿巩固治疗后的可测量残留疾病结果有用吗?
在急性淋巴细胞白血病(ALL)患儿首次巩固治疗(EOC)结束后的晚期时间点定期检测可测量残留病(MRD)。问题是这是否有助于检测(分子)复发。我们研究了接受DCOG-ALL-10(n = 271)和DCOG-ALL-9(n = 122)治疗的中危患者在EOC后MRD的临床意义,这些患者在EOC时MRD为0.05%。无论后期时间点的MRD结果如何,EOC MRD阴性患者(n = 178)的预后都很好;所有后期时间点MRD阴性的患者6年累积复发率(6-y CIR)为7.4%(95% CI,3.9%-12.3%),而一个或多个后期时间点MRD阳性的患者6年累积复发率(6-y CIR)为3.8%(95% CI,0.3%-16.8%)(p = 0.51)。MRD 阳性的 EOC 患者(n = 91)中,随后的时间点为 MRD 阴性的患者(n = 43)的预后相当好,6 年 CIR 为 7.0% (95% CI, 1.8%-17.2%) 。相比之下,EOC时MRD阳性且随后一个或多个时间点MRD阳性的患者(n = 48)复发风险更高,6年CIR为29.4%(95% CI,17.2%-42.8%),p <0.001。这些发现在ALL-9的验证队列中以及使用更新的EuroMRD指南中得到了证实。对于EOC MRD阴性患者,可以放弃后续的MRD测量。对于EOC MRD阳性患者,后续的MRD测量可能有助于进一步的风险分层。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Leukemia
医学-血液学
CiteScore
18.10
自引率
3.50%
发文量
270
审稿时长
3-6 weeks
期刊介绍:
Title: Leukemia
Journal Overview:
Publishes high-quality, peer-reviewed research
Covers all aspects of research and treatment of leukemia and allied diseases
Includes studies of normal hemopoiesis due to comparative relevance
Topics of Interest:
Oncogenes
Growth factors
Stem cells
Leukemia genomics
Cell cycle
Signal transduction
Molecular targets for therapy
And more
Content Types:
Original research articles
Reviews
Letters
Correspondence
Comments elaborating on significant advances and covering topical issues
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


