Mosaic chromosomal alterations in hematopoietic cells and clinical outcomes in patients with multiple myeloma
IF 12.8
1区 医学
Q1 HEMATOLOGY
引用次数: 0
Abstract
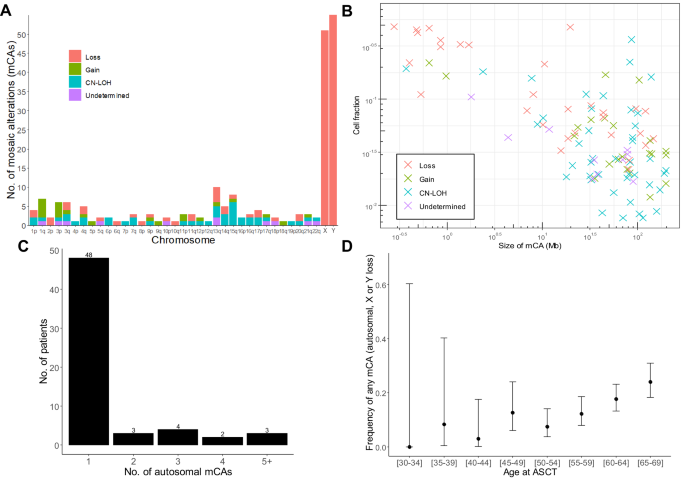
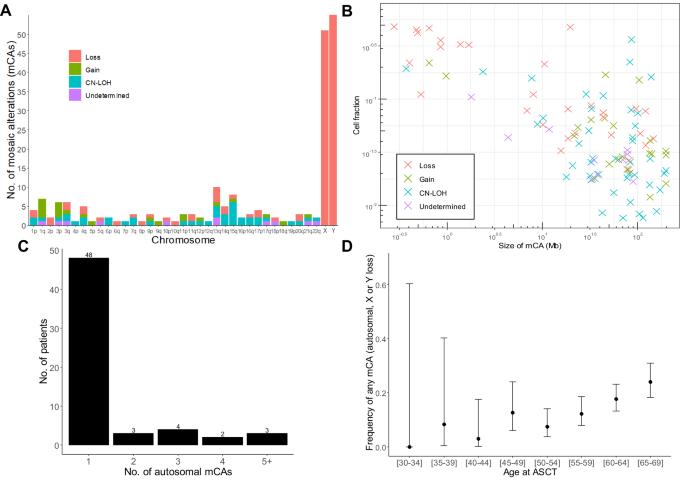
Mosaic chromosomal alterations (mCAs) in hematopoietic cells increase mortality and risk of hematological cancers and infections. We investigated the landscape of mCAs and their clinical consequences in 976 patients with multiple myeloma undergoing high-dose chemotherapy and autologous stem cell support (ASCT) with median 6.4 years of follow-up. mCAs were detected in the stem cell harvest product of 158 patients (16.2%). Autosomal aberrations were found in 60 patients (6.1%) and affected all chromosomes. Loss of chromosome X was found in 51 females (12.7%) and loss of chromosome Y in 55 males (9.6%). Overall survival and progression were similar between carriers of autosomal mCAs and non-carriers. In contrast, female patients with loss of the X chromosome had longer overall survival (age-adjusted[a.a.] HR 0.54, 95% CI 0.32–0.93, p = 0.02), lower risk of progression (a.a. HR 0.55, 95% CI 0.35–0.87; p = 0.01), and better post-transplant response (higher degree of complete response (CR) or very good partial response (VGPR)). The reason for this substantial effect is unknown. Additionally, myeloma clones in the stem cell product was confirmed by mCA analysis in the few patients with multiple mCAs (n = 12 patients). Multiple mCAs conferred inferior overall survival (a.a. HR 2.0, 95% CI 1.02–3.84; p = 0.04) and higher risk of myeloma progression (a.a. HR 3.36, 95% CI 1.67–6.81; p < 0.001), which is presumed to be driven by suspected myeloma contaminants.
多发性骨髓瘤患者造血细胞中的染色体镶嵌改变与临床预后。
造血细胞中的镶嵌染色体改变(mCAs)会增加死亡率以及罹患血癌和感染的风险。我们调查了976名接受大剂量化疗和自体干细胞支持(ASCT)的多发性骨髓瘤患者的mCAs情况及其临床后果,中位随访时间为6.4年。60名患者(6.1%)发现常染色体畸变,影响所有染色体。51名女性(12.7%)发现X染色体缺失,55名男性(9.6%)发现Y染色体缺失。常染色体 mCAs 携带者与非携带者的总体生存期和病情进展相似。相比之下,X 染色体缺失的女性患者总生存期更长(年龄调整[a.a.] HR 0.54,95% CI 0.32-0.93,p = 0.02),病情进展风险更低(a.a.HR 0.55,95% CI 0.35-0.87;p = 0.01),移植后反应更好(完全反应(CR)或非常好的部分反应(VGPR)程度更高)。这种实质性影响的原因尚不清楚。此外,干细胞产物中的骨髓瘤克隆在少数有多个mCA的患者(12人)中通过mCA分析得到证实。多发性mCA导致总生存率降低(a.a. HR 2.0, 95% CI 1.02-3.84; p = 0.04)和骨髓瘤进展风险升高(a.a. HR 3.36, 95% CI 1.67-6.81; p = 0.04)。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Leukemia
医学-血液学
CiteScore
18.10
自引率
3.50%
发文量
270
审稿时长
3-6 weeks
期刊介绍:
Title: Leukemia
Journal Overview:
Publishes high-quality, peer-reviewed research
Covers all aspects of research and treatment of leukemia and allied diseases
Includes studies of normal hemopoiesis due to comparative relevance
Topics of Interest:
Oncogenes
Growth factors
Stem cells
Leukemia genomics
Cell cycle
Signal transduction
Molecular targets for therapy
And more
Content Types:
Original research articles
Reviews
Letters
Correspondence
Comments elaborating on significant advances and covering topical issues
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


