Gastrointestinal involvement refines prognosis in minnesota standard risk acute graft-vs.-host disease
IF 4.5
2区 医学
Q1 HEMATOLOGY
引用次数: 0
Abstract
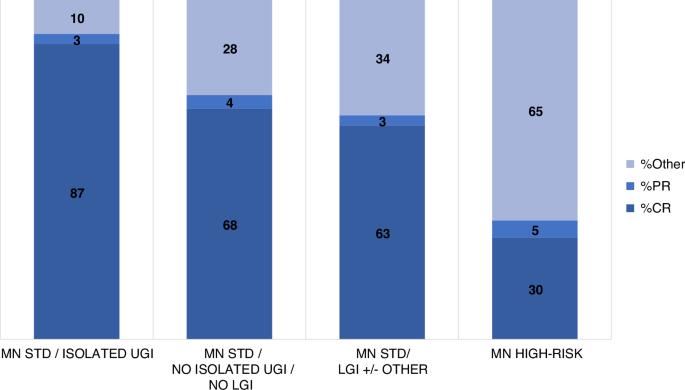
Minnesota acute graft versus host disease (AGVHD) risk score is a validated tool to stratify newly-diagnosed patients into standard-risk (SR) and high-risk (HR) groups with ~85% having SR AGVHD. We aimed to identify factors for further risk-stratification within Minnesota SR patients. A single-center, retrospective analysis of consecutive patients between 1/2010 and 12/2014 was performed. Patients who developed AGVHD within 100 days and treated with systemic corticosteroids were included (N = 416), 356 (86%) of which were Minnesota SR and 60 (14%) had HR AGVHD. Isolated upper gastrointestinal (GI) AGVHD patients had significantly better day 28 and 56 CR/PR rates (90% vs. 72%, p = 0.004) and (83% vs 66%, p = 0.01), respectively, and lower 1-year non-relapse mortality (NRM; 10% vs. 22%; HR 0.4, p = 0.03). Lower GI AGVHD had less favorable outcomes with 1-year NRM of 40% (HR 2.1, p = 0.001), although CR/PR rates were not statistically different. In multivariate analysis, lower GI involvement (HR 2.6, p < 0.001), age ≥ 50 (HR 2.9, p < 0.001) and HCT-CI > 3 (HR 2.1, p = 0.002) predicted for 1-year NRM. Heterogeneity within Minnesota SR patients requires consideration in clinical trials, as distinct outcomes are observed in those with isolated upper GI and lower GI AGVHD, highlighting the importance of stratification in clinical trial design.
胃肠道受累使明尼苏达州标准风险急性移植物抗宿主病的预后得到改善。
明尼苏达州急性移植物抗宿主疾病(AGVHD)风险评分是将新诊断患者分为标准风险(SR)组和高风险(HR)组的有效工具,其中约 85% 的患者为 SR AGVHD。我们旨在确定在明尼苏达州 SR 患者中进一步进行风险分层的因素。我们对 2010 年 1 月至 2014 年 12 月期间的连续患者进行了单中心回顾性分析。纳入了在 100 天内发生 AGVHD 并接受全身皮质类固醇治疗的患者(N = 416),其中 356 例(86%)为明尼苏达州 SR,60 例(14%)为 HR AGVHD。孤立的上消化道 (GI) AGVHD 患者第 28 天和第 56 天的 CR/PR 率分别显著提高(90% vs. 72%,p = 0.004)和(83% vs. 66%,p = 0.01),1 年非复发死亡率(NRM;10% vs. 22%;HR 0.4,p = 0.03)也较低。下消化道AGVHD的预后较差,1年非复发死亡率为40%(HR 2.1,p = 0.001),但CR/PR率没有统计学差异。在多变量分析中,较低的胃肠道受累(HR 2.6,p = 0.002)可预测 1 年的 NRM。明尼苏达州SR患者的异质性需要在临床试验中加以考虑,因为在孤立的上消化道和下消化道AGVHD患者中观察到了不同的结果,这凸显了临床试验设计中分层的重要性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Bone Marrow Transplantation
医学-免疫学
CiteScore
8.40
自引率
8.30%
发文量
337
审稿时长
6 months
期刊介绍:
Bone Marrow Transplantation publishes high quality, peer reviewed original research that addresses all aspects of basic biology and clinical use of haemopoietic stem cell transplantation.
The broad scope of the journal thus encompasses topics such as stem cell biology, e.g., kinetics and cytokine control, transplantation immunology e.g., HLA and matching techniques, translational research, and clinical results of specific transplant protocols. Bone Marrow Transplantation publishes 24 issues a year.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


