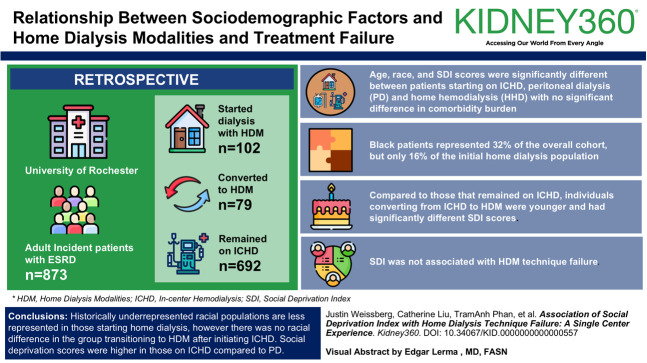
Association of Social Deprivation Index with Home Dialysis Technique Failure: A Single-Center Experience.
IF 3
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
社会贫困指数与家庭透析技术失败的关系:单中心经验。
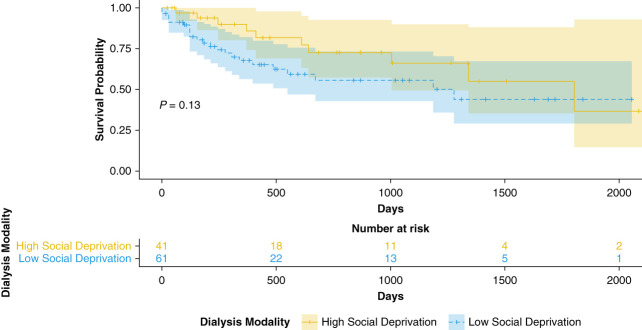
背景:尽管家庭透析(HDM)为患者和医疗保健系统带来了诸多好处,但其利用率仍然很低,尤其是在少数种族和少数民族以及社会人口压力较大的人群中。医疗服务提供者对不良后果和家庭透析失败的担忧仍然是家庭透析转诊的一个障碍。我们调查了社会人口因素与使用 HDM 和技术失败之间的关系:我们对罗切斯特大学六年内的成年 ESRD 患者进行了一项回顾性队列研究,以评估人口统计因素、社会贫困指数 (SDI) 和并发症负担与使用 HDM 和技术失败之间的关系。通过计算个人时间发病率来比较结果变量,并使用泊松率比检验来比较发病率。采用单变量考克斯回归法研究影响技术失败的预测因素:在 873 名患者中,102 人开始使用 HDM 透析,79 人转为 HDM 透析,692 人继续使用中心内血液透析 (ICHD)。开始接受中心内血液透析(ICHD)、腹膜透析(PD)和家庭血液透析(HHD)的患者在年龄、种族和 SDI 评分方面存在显著差异,但在合并症负担方面没有显著差异。黑人患者占整个群体的 32%,但只占初始家庭透析患者的 16%。与仍在接受 ICHD 的患者相比,从 ICHD 转为 HDM 的患者更年轻,其 SDI 评分也有显著差异。SDI与HDM技术失败无关:结论:在开始进行家庭透析的人群中,历来代表性不足的种族人口比例较低,但在开始进行 ICHD 后转为 HDM 的人群中没有种族差异。与透析患者相比,接受 ICHD 患者的社会贫困程度得分更高。社会贫困程度和种族都不能预测家庭治疗的成功率。这些研究结果表明了初始模式的差异,以及与使用家庭透析相关的社会人口因素与预测 HDM 技术失败的社会人口因素之间的脱节。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


