Clinical outcomes of MAFLD versus NAFLD: A meta-analysis of observational studies
Abstract
Importance
The recent change in terminology from nonalcoholic fatty liver disease (NAFLD) to metabolic dysfunction-associated fatty liver disease (MAFLD) and metabolic dysfunction-associated steatotic liver disease (MASLD) highlights the link between hepatic steatosis and metabolic dysfunction, taking out the stigmata of alcohol.
Objective
We compared the effects of NAFLD and MAFLD definitions on the risk of overall and cardiovascular (CV) mortality, liver-related events (LRE), nonfatal CV events (CVE), chronic kidney disease (CKD), and extra-hepatic cancers (EHC).
Data Sources and Study Selection
We systematically searched four large electronic databases for cohort studies (published through August 2023) that simultaneously used NAFLD and MAFLD definitions for examining the risk of mortality and adverse CV, renal, or oncological outcomes associated with both definitions. In total, 21 eligible cohort studies were identified. Meta-analysis was performed using random-effects modelling.
Results
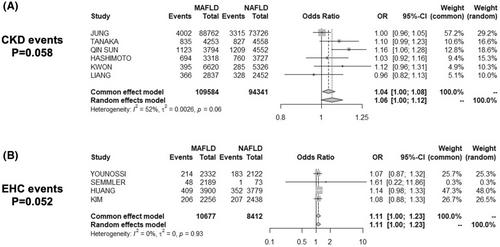
Compared with those with NAFLD, individuals with MAFLD had significantly higher rates of overall mortality (random-effect OR 1.12, 95% CI 1.04–1.21, p = .004) and CV mortality (random-effect OR 1.15, 95% CI 1.04–1.26, p = .004), and a marginal trend towards higher rates of developing CKD (random-effect OR 1.06, 95% CI 1.00–1.12, p = .058) and EHC events (random-effect OR 1.11, 95% CI 1.00–1.23, p = .052). We found no significant differences in the risk LREs and nonfatal CVE between MAFLD and NAFLD. Meta-regression analyses identified male sex and metabolic comorbidities as the strongest risk factors related to the risk of adverse clinical outcomes in MAFLD compared to NAFLD.
Conclusions and Relevance
Individuals with MAFLD have higher rates of overall and CV mortality and higher rates of developing CKD and EHC events than those with NAFLD, possibly due to the dysmetabolic risk profile related to MAFLD.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


