Cost-effectiveness of point of care smoking cessation interventions in oncology clinics
IF 6.4
1区 医学
Q1 ONCOLOGY
引用次数: 0
Abstract
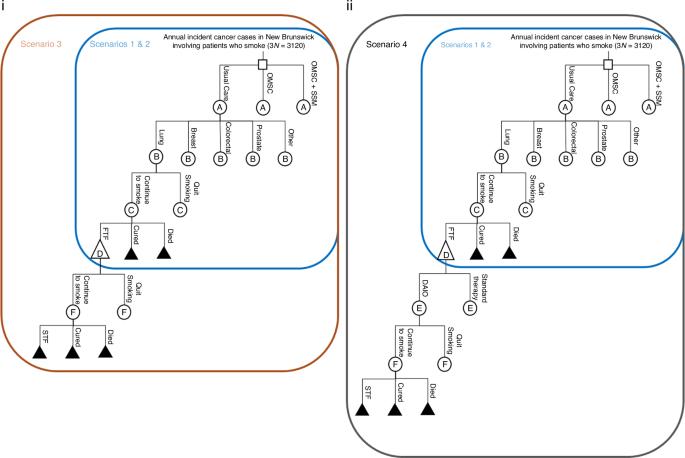
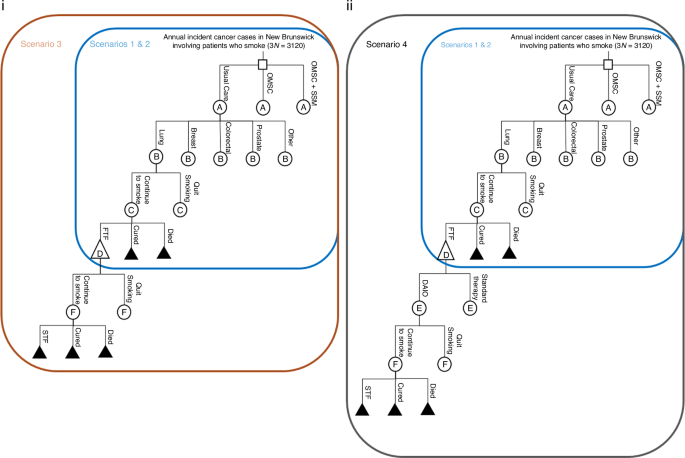
We examined the cost-effectiveness of providing systematic smoking cessation interventions to oncology patients at point-of-care. A decision analytic model was completed from the healthcare payer’s perspective and included all incident cancer cases involving patients who smoke in New Brunswick, Canada (n = 1040), cancer site stratifications, and risks of mortality, continued smoking, and cancer treatment failure over one year. Usual care (no cessation support) was compared to the standard Ottawa Model for Smoking Cessation (OMSC) intervention, and to OMSC plus unlimited cost-free stop smoking medication (OMSC + SSM), including nicotine replacement therapy, varenicline, or bupropion. Primary outcomes were incremental cost per quit (ICQ) and incremental cost per cancer treatment failure avoided (ICTFA). The ICQ was $C143 and ICTFA $C1193 for standard OMSC. The ICQ was $C503 and ICTFA was $C5952 for OMSC + SSM. The number needed to treat (NNT) to produce one quit was 9 for standard OMSC and 4 for OMSC + SSM, and the NNT to avoid one first-line treatment failure was 78 for OMSC and 45 for OMSC + SSM. Both were cost-effective in 100% of 1000 simulations. Given the high clinical benefits and low incremental costs, systematic smoking cessation interventions should be a standard component of first-line cancer treatment.
肿瘤诊所戒烟治疗点干预的成本效益。
背景我们研究了在护理点为肿瘤患者提供系统戒烟干预的成本效益:方法:我们从医疗支付方的角度建立了一个决策分析模型,其中包括加拿大新不伦瑞克省所有涉及吸烟患者的癌症病例(n = 1040)、癌症部位分层以及一年内的死亡风险、继续吸烟风险和癌症治疗失败风险。将常规护理(无戒烟支持)与标准的渥太华戒烟模式(OMSC)干预进行了比较,还将其与OMSC加无限量免费戒烟药物(OMSC + SSM)(包括尼古丁替代疗法、伐尼克兰或安非他明)进行了比较。主要结果是每次戒烟的增量成本(ICQ)和每次避免癌症治疗失败的增量成本(ICTFA):结果:标准 OMSC 的 ICQ 为 143 美元,ICTFA 为 1193 美元。OMSC + SSM的ICQ为503美元,ICTFA为5952美元。标准 OMSC 和 OMSC + SSM 产生一次戒断所需的治疗次数(NNT)分别为 9 和 4,OMSC 和 OMSC + SSM 避免一次一线治疗失败所需的 NNT 分别为 78 和 45。在 1000 次模拟测试中,两者的成本效益均为 100%:鉴于临床疗效高、增量成本低,系统性戒烟干预应成为癌症一线治疗的标准组成部分。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

British Journal of Cancer
医学-肿瘤学
CiteScore
15.10
自引率
1.10%
发文量
383
审稿时长
6 months
期刊介绍:
The British Journal of Cancer is one of the most-cited general cancer journals, publishing significant advances in translational and clinical cancer research.It also publishes high-quality reviews and thought-provoking comment on all aspects of cancer prevention,diagnosis and treatment.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


