Distinct effects of intravenous bone marrow-derived mesenchymal stem cell therapy on ischemic and non-ischemic lungs after ischemia-reperfusion injury
IF 3.7
3区 医学
Q2 BIOTECHNOLOGY & APPLIED MICROBIOLOGY
引用次数: 0
Abstract
Background
The preclinical efficacy of mesenchymal stem cell (MSC) therapy after intravenous infusion has been promising, but clinical studies have yielded only modest results. Although most preclinical studies have focused solely on the ischemic lung, it is crucial to evaluate both lungs after ischemia-reperfusion injury, considering the various mechanisms involved. This study aimed to bridge this gap by assessing the acute effects of bone marrow MSC(BM) infusion before ischemic insult and evaluating both ischemic and non-ischemic lungs after reperfusion.
Methods
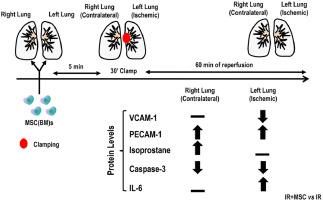
Eighteen male Wistar rats (403 ± 23 g) were anesthetized and mechanically ventilated using a protective strategy. After baseline data collection, the animals were randomized to 3 groups (n = 6/group): (1) SHAM; (2) ischemia-reperfusion (IR), and (3) intravenous MSC(BM) infusion followed by IR. Ischemia was induced by complete clamping of the left hilum, followed by 1 h of reperfusion after clamp removal. At the end of the experiment, the right and left lungs (non-ischemic and ischemic, respectively) were collected for immunohistochemistry and molecular biology analysis.
Results
MSC(BM)s reduced endothelial cell damage and apoptosis markers and improved markers associated with endothelial cell integrity in both lungs. In addition, gene expression of catalase and nuclear factor erythroid 2-related factor 2 increased after MSC(BM) therapy. In the ischemic lung, MSC(BM) therapy mitigated endothelial cell damage and apoptosis and increased gene expression associated with endothelial cell integrity. Conversely, in the non-ischemic lung, apoptosis gene expression increased in the IR group but not after MSC(BM) therapy.
Conclusion
This study demonstrates distinct effects of MSC(BM) therapy on ischemic and non-ischemic lungs after ischemia-reperfusion injury. The findings underscore the importance of evaluating both lung types in ischemia-reperfusion studies, offering insights into the therapeutic potential of MSC(BM) therapy in the context of lung injury.
静脉注射骨髓间充质干细胞疗法对缺血再灌注损伤后缺血肺和非缺血肺的不同影响
背景间充质干细胞(MSC)静脉注射后的临床前疗效令人鼓舞,但临床研究结果却不尽人意。虽然大多数临床前研究只关注缺血肺,但考虑到缺血再灌注损伤的各种机制,对缺血再灌注损伤后的双肺进行评估至关重要。本研究旨在通过评估骨髓间充质干细胞(BM)在缺血损伤前输注的急性效应以及再灌注后缺血和非缺血肺的评估来弥补这一差距。收集基线数据后,将动物随机分为 3 组(n = 6/组):(1) SHAM;(2) 缺血再灌注(IR);(3) 静脉输注间充质干细胞(BM)后再进行 IR。缺血是通过完全钳夹左侧肝脏诱发的,然后在钳夹移除后再灌注 1 小时。实验结束后,收集右肺和左肺(分别为非缺血肺和缺血肺)进行免疫组化和分子生物学分析。此外,间充质干细胞(BM)治疗后,过氧化氢酶和核因子红细胞2相关因子2的基因表达增加。在缺血肺中,间充质干细胞(BM)疗法减轻了内皮细胞损伤和凋亡,增加了与内皮细胞完整性相关的基因表达。结论:这项研究显示了间充质干细胞(BM)疗法对缺血再灌注损伤后缺血肺和非缺血肺的不同影响。这些发现强调了在缺血再灌注研究中评估两种肺类型的重要性,为间叶干细胞(BM)疗法在肺损伤中的治疗潜力提供了启示。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Cytotherapy
医学-生物工程与应用微生物
CiteScore
6.30
自引率
4.40%
发文量
683
审稿时长
49 days
期刊介绍:
The journal brings readers the latest developments in the fast moving field of cellular therapy in man. This includes cell therapy for cancer, immune disorders, inherited diseases, tissue repair and regenerative medicine. The journal covers the science, translational development and treatment with variety of cell types including hematopoietic stem cells, immune cells (dendritic cells, NK, cells, T cells, antigen presenting cells) mesenchymal stromal cells, adipose cells, nerve, muscle, vascular and endothelial cells, and induced pluripotential stem cells. We also welcome manuscripts on subcellular derivatives such as exosomes. A specific focus is on translational research that brings cell therapy to the clinic. Cytotherapy publishes original papers, reviews, position papers editorials, commentaries and letters to the editor. We welcome "Protocols in Cytotherapy" bringing standard operating procedure for production specific cell types for clinical use within the reach of the readership.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


