Efficacy and safety of pulsed-field versus conventional thermal ablation for atrial fibrillation: A systematic review and meta-analysis
Abstract
Background
Pulsed-field ablation (PFA) has emerged as an innovative alternative to radiofrequency (RF) and cryoablation because it selectively targets myocardial tissue. Thus, we aim to estimate the efficacy and safety of PFA versus thermal ablation for atrial fibrillation (AF) ablation.
Methods
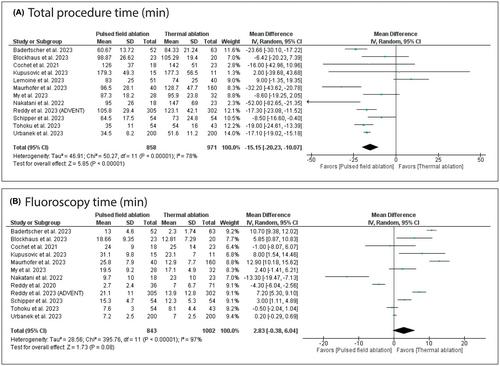
A systematic review and meta-analysis were retrieved from PubMed, WOS, SCOPUS, EMBASE, and CENTRAL through September 2023. We used RevMan V. 5.4 to pool dichotomous data using risk ratio (RR) and continuous data using mean difference (MD) with a 95% confidence interval (CI). PROSPERO ID: CRD42023480321
Results
We included 17 studies with a total of 2255 patients. PFA was significantly associated with a decreased incidence of AF recurrence (RR: 0.66 with 95% CI [0.51, 0.87], p = .003). However, there was no significant difference between PFA and thermal ablation in arrhythmia recurrence (RR: 0.92 with 95% CI [0.74, 1.46], p = .42). PFA was significantly associated with decreased total procedure time (MD: −15.15 with 95% CI [−20.23, −10.07], p < .00001), decreased heart rate change (MD: −7.39 with 95% CI [−12.16, −2.62], p = .002), decreased phrenic nerve palsy (RR: 0.38 with 95% CI [0.15, 0.98], p = .05), and reduced esophageal lesions (RR: 0.09 with 95% CI [0.01, 0.69], p = .02). On the contrary, PFA was significantly associated with increased pericardial tamponade (RR: 6.14 with 95% CI [1.43, 26.33], p = .01).
Conclusion
PFA was significantly associated with decreased AF recurrence, total procedure time, heart rate change, phrenic nerve palsy, esophageal lesion, and increased incidence of pericardial tamponade compared with thermal ablation.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


