Implementing a male-specific ART counselling curriculum: a quality assessment with healthcare workers in Malawi
Abstract
Introduction
There is little HIV counselling that directly meets the needs of men in Eastern and Southern Africa, limiting men's knowledge about the benefits of HIV treatment and how to overcome barriers to engagement, contributing to poorer HIV-related outcomes than women. Male-specific approaches are needed to improve men's outcomes but may be difficult for healthcare workers (HCWs) to implement with fidelity and quality in low-resource settings. We developed a male-specific counselling curriculum which was implemented by male HCWs and then conducted a mixed-methods quality assessment.
Methods
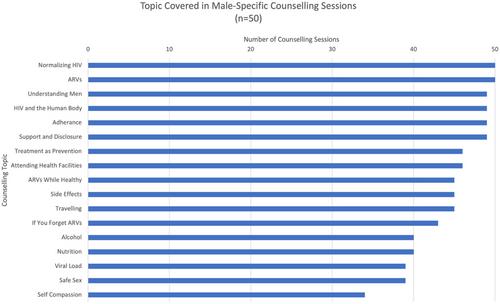
We audio-recorded counselling sessions to assess the quality of implementation (n = 50) by male HCWs from two cadres (nurse, n = 10 and lay cadre, n = 10) and conducted focus group discussions (FGDs) with HCWs at 6 and 9 months after rollout to understand barriers and facilitators to implementation. Counselling sessions and FGDs were translated, transcribed and analysed using thematic analysis adapted from WHO Quality Counselling Guidelines. We assessed if sessions were respectful, informative, interactive, motivating and included tailored action plans for overcoming barriers to care. All data were collected September 2021−June 2022.
Results
All sessions used respectful, non-judgemental language. Sessions were highly interactive with most HCWs frequently asking open-ended questions (n = 46, 92%) and often incorporating motivational explanations of how antiretroviral therapy contributes to life goals (n = 42, 84%). Few sessions included individually tailored action plans for clients to overcome barriers to care (n = 9, 18%). New counselling themes were well covered; however, occasionally themes of self-compassion and safe sex were not covered during sessions (n = 16 and n = 11). HCWs believed that having male HCWs conduct counselling, ongoing professional development and keeping detailed counselling notes facilitated quality implementation. Perceived barriers included curriculum length and client hesitancy to participate in action plan development. Findings were similar across cadres.
Conclusions
Implementing high-quality male-specific counselling using male nurses and/or lay cadre is feasible. Efforts to utilize lay cadres should be prioritized, particularly in low-resource settings. Programmes should provide comprehensive job aids to support HCWs. Ongoing training and professional development are needed to (1) improve HCWs’ skills in tailored action plans, and (2) sensitize HCWs to the need for self-compassion within male clients to promote holistic sexual health.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


