Associations of diabetes and mortality among colorectal cancer patients from the Southern Community Cohort Study
IF 6.4
1区 医学
Q1 ONCOLOGY
引用次数: 0
Abstract
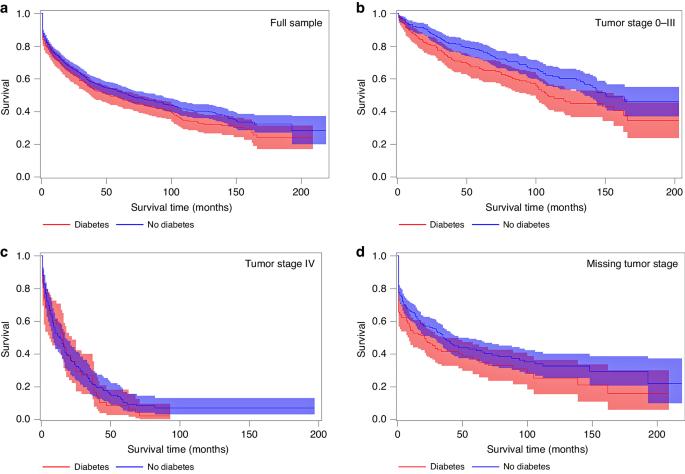
We investigated associations between diabetes and mortality among participants with incident colorectal cancer (CRC) from the Southern Community Cohort Study. Participants (73% non-Hispanic Black; 60% income < $15,000) were recruited between 2002–2009. Diabetes was self-reported at enrollment and follow-up surveys at approximately 5-year intervals. Incident CRC and mortality were identified via state registries and the National Death Index. Proportional hazards models calculated associations between diabetes with overall, CRC-specific mortality among 1059 participants with incident CRC. Diabetes prior to diagnosis is associated with elevated overall (hazard ratio [95% confidence interval]: (1.46[1.22–1.75]), and CRC-specific mortality (1.36[1.06–1.74])) after adjustment for tumor stage. For non-Hispanic Black and non-Hispanic White participants, consistent associations were observed for overall (1.35[1.10–1.66] vs. 1.89[1.31–2.72], respectively, p-interaction = 0.11) and CRC-specific mortality (1.30[0.99–1.71] vs. 1.77[1.06–2.95], respectively, p-interaction = 0.28). For individuals with incomes <$15,000/year, associations with overall (1.44[1.15–1.79]) and CRC-specific mortality (1.28[0.94–1.73]) were similar to the full sample. Associations with overall (1.71[1.37–2.13]) and CRC-specific mortality (1.65[1.22–2.22]) were highest for diabetes ≥ 10 years at diagnosis. Pre-diagnosis diabetes is associated with higher mortality among participants with incident CRC from a predominantly non-Hispanic Black cohort with lower socioeconomic status. The higher prevalence of diabetes in this population may contribute to racial disparities in CRC mortality.
南方社区队列研究》中结直肠癌患者的糖尿病与死亡率之间的关系。
背景:我们调查了南方社区队列研究(Southern Community Cohort Study)中患有结直肠癌(CRC)的参与者中糖尿病与死亡率之间的关系:方法:参与者(73% 为非西班牙裔黑人;60% 为收入 结果:诊断前患糖尿病与总死亡率的升高有关(从 0.2% 升至 0.5%):经肿瘤分期调整后,诊断前糖尿病与总体死亡率(危险比[95% 置信区间]:1.46[1.22-1.75])和 CRC 特异性死亡率(1.36[1.06-1.74])升高有关。在非西班牙裔黑人和非西班牙裔白人参与者中,总体死亡率(分别为 1.35[1.10-1.66] vs. 1.89[1.31-2.72],p-交互作用 = 0.11)和 CRC 特异性死亡率(分别为 1.30[0.99-1.71] vs. 1.77[1.06-2.95],p-交互作用 = 0.28)的相关性一致。对于有收入的人 结论:诊断前糖尿病与癌症特异性死亡率相关:在社会经济地位较低的非西班牙裔黑人队列中,诊断前糖尿病与较高的 CRC 患者死亡率相关。该人群中较高的糖尿病患病率可能会导致 CRC 死亡率的种族差异。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
British Journal of Cancer
医学-肿瘤学
CiteScore
15.10
自引率
1.10%
发文量
383
审稿时长
6 months
期刊介绍:
The British Journal of Cancer is one of the most-cited general cancer journals, publishing significant advances in translational and clinical cancer research.It also publishes high-quality reviews and thought-provoking comment on all aspects of cancer prevention,diagnosis and treatment.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


