Estimating the potential value of MSM-focused evidence-based implementation interventions in three Ending the HIV Epidemic jurisdictions in the United States: a model-based analysis
Abstract
Introduction
Improving the delivery of existing evidence-based interventions to prevent and diagnose HIV is key to Ending the HIV Epidemic in the United States. Structural barriers in the access and delivery of related health services require municipal or state-level policy changes; however, suboptimal implementation can be addressed directly through interventions designed to improve the reach, effectiveness, adoption or maintenance of available interventions. Our objective was to estimate the cost-effectiveness and potential epidemiological impact of six real-world implementation interventions designed to address these barriers and increase the scale of delivery of interventions for HIV testing and pre-exposure prophylaxis (PrEP) in three US metropolitan areas.
Methods
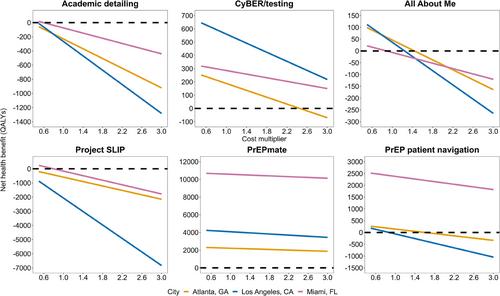
We used a dynamic HIV transmission model calibrated to replicate HIV microepidemics in Atlanta, Los Angeles (LA) and Miami. We identified six implementation interventions designed to improve HIV testing uptake (“Academic detailing for HIV testing,” “CyBER/testing,” “All About Me”) and PrEP uptake/persistence (“Project SLIP,” “PrEPmate,” “PrEP patient navigation”). Our comparator scenario reflected a scale-up of interventions with no additional efforts to mitigate implementation and structural barriers. We accounted for potential heterogeneity in population-level effectiveness across jurisdictions. We sustained implementation interventions over a 10-year period and evaluated HIV acquisitions averted, costs, quality-adjusted life years and incremental cost-effectiveness ratios over a 20-year time horizon (2023–2042).
Results
Across jurisdictions, implementation interventions to improve the scale of HIV testing were most cost-effective in Atlanta and LA (CyBER/testing cost-saving and All About Me cost-effective), while interventions for PrEP were most cost-effective in Miami (two of three were cost-saving). We estimated that the most impactful HIV testing intervention, CyBER/testing, was projected to avert 111 (95% credible interval: 110–111), 230 (228–233) and 101 (101–103) acquisitions over 20 years in Atlanta, LA and Miami, respectively. The most impactful implementation intervention to improve PrEP engagement, PrEPmate, averted an estimated 936 (929–943), 860 (853–867) and 2152 (2127–2178) acquisitions over 20 years, in Atlanta, LA and Miami, respectively.
Conclusions
Our results highlight the potential impact of interventions to enhance the implementation of existing evidence-based interventions for the prevention and diagnosis of HIV.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


