Intervention strategies to improve adherence to treatment for selected chronic conditions in sub-Saharan Africa: a systematic review
Abstract
Introduction
Evidence-based intervention strategies to improve adherence among individuals living with chronic conditions are critical in ensuring better outcomes. In this systematic review, we assessed the impact of interventions that aimed to promote adherence to treatment for chronic conditions.
Methods
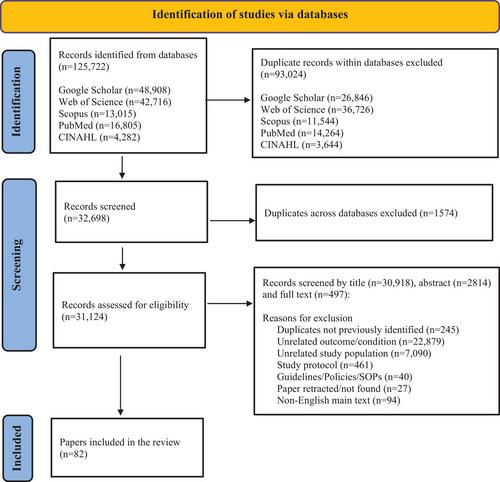
We systematically searched PubMed, Web of Science, Scopus, Google Scholar and CINAHL databases to identify relevant studies published between the years 2000 and 2023 and used the QUIPS assessment tool to assess the quality and risk of bias of each study. We extracted data from eligible studies for study characteristics and description of interventions for the study populations of interest.
Results
Of the 32,698 total studies/records screened, 2814 were eligible for abstract screening and of those, 497 were eligible for full-text screening. A total of 82 studies were subsequently included, describing a total of 58,043 patients. Of the total included studies, 58 (70.7%) were related to antiretroviral therapy for HIV, 6 (7.3%) were anti-hypertensive medication-related, 12 (14.6%) were anti-diabetic medication-related and 6 (7.3%) focused on medication for more than one condition. A total of 54/82 (65.9%) reported improved adherence based on the described study outcomes, 13/82 (15.9%) did not have clear results or defined outcomes, while 15/82 (18.3%) reported no significant difference between studied groups. The 82 publications described 98 unique interventions (some studies described more than one intervention). Among these intervention strategies, 13 (13.3%) were multifaceted (4/13 [30.8%] multi-component health services- and community-based programmes, 6/13 [46.2%] included individual plus group counselling and 3/13 [23.1%] included SMS or alarm reminders plus individual counselling).
Discussion
The interventions described in this review ranged from adherence counselling to more complex interventions such as mobile health (mhealth) interventions. Combined interventions comprised of different components may be more effective than using a single component in isolation. However, the complexity involved in designing and implementing combined interventions often complicates the practicalities of such interventions.
Conclusions
There is substantial evidence that community- and home-based interventions, digital health interventions and adherence counselling interventions can improve adherence to medication for chronic conditions. Future research should answer if existing interventions can be used to develop less complicated multifaceted adherence intervention strategies.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


