Extracellular vesicles from type-2 macrophages increase the survival of chronic lymphocytic leukemia cells ex vivo
IF 4.8
3区 医学
Q1 BIOTECHNOLOGY & APPLIED MICROBIOLOGY
引用次数: 0
Abstract
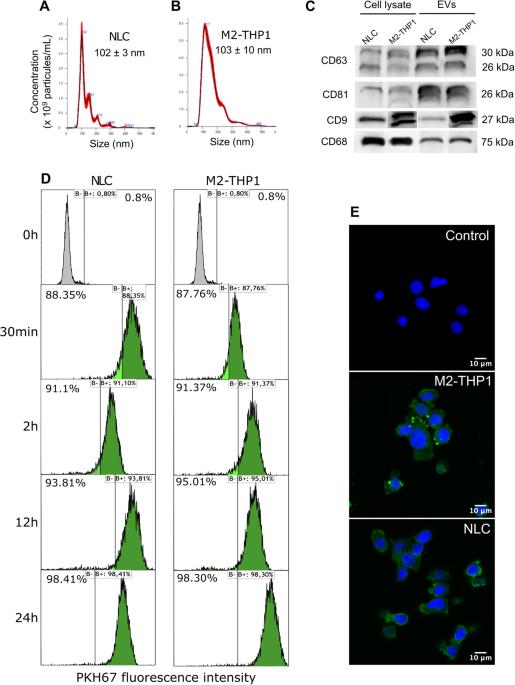
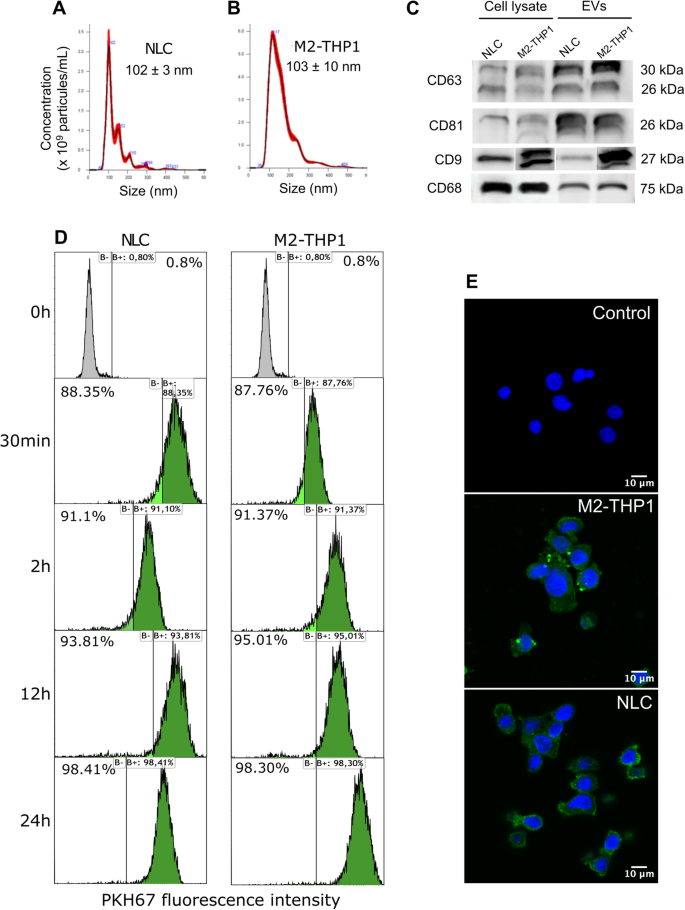
The resistance of Chronic Lymphocytic Leukemia (CLL) B-cells to cell death is mainly attributed to interactions within their microenvironment, where they interact with various types of cells. Within this microenvironment, CLL-B-cells produce and bind cytokines, growth factors, and extracellular vesicles (EVs). In the present study, EVs purified from nurse-like cells and M2-polarized THP1 cell (M2-THP1) cultures were added to CLL-B-cells cultures. EVs were rapidly internalized by B-cells, leading to a decrease in apoptosis (P = 0.0162 and 0.0469, respectively) and an increased proliferation (P = 0.0335 and 0.0109). Additionally, they induced an increase in the resistance of CLL-B-cells to Ibrutinib, the Bruton kinase inhibitor in vitro (P = 0.0344). A transcriptomic analysis showed an increase in the expression of anti-apoptotic gene BCL-2 (P = 0.0286) but not MCL-1 and an increase in the expression of proliferation-inducing gene APRIL (P = 0.0286) following treatment with EVs. Meanwhile, an analysis of apoptotic protein markers revealed increased amounts of IGFBP-2 (P = 0.0338), CD40 (P = 0.0338), p53 (P = 0.0219) and BCL-2 (P = 0.0338). Finally, exploration of EVs protein content by mass spectrometry revealed they carry various proteins involved in known oncogenic pathways and the RNAseq analysis of CLL-B-cells treated or not with NLCs EVs show various differentially expressed genes.
来自 2 型巨噬细胞的细胞外囊泡可提高慢性淋巴细胞白血病细胞的体内存活率。
慢性淋巴细胞性白血病(CLL)B 细胞对细胞死亡的抵抗力主要归因于其微环境中的相互作用,它们在微环境中与各种类型的细胞相互作用。在这种微环境中,CLL-B 细胞产生并结合细胞因子、生长因子和细胞外囊泡 (EV)。在本研究中,将从护士样细胞和 M2 极化 THP1 细胞(M2-THP1)培养物中纯化的 EVs 添加到 CLL-B 细胞培养物中。EVs 被 B 细胞快速内化,导致细胞凋亡减少(P = 0.0162 和 0.0469)和增殖增加(P = 0.0335 和 0.0109)。此外,它们还诱导增加了CLL-B细胞对体外布鲁顿激酶抑制剂伊布替尼(Ibrutinib)的耐药性(P = 0.0344)。转录组分析表明,用EVs处理后,抗凋亡基因BCL-2的表达增加(P = 0.0286),但MCL-1没有增加;增殖诱导基因APRIL的表达增加(P = 0.0286)。同时,对凋亡蛋白标记物的分析表明,IGFBP-2(P = 0.0338)、CD40(P = 0.0338)、p53(P = 0.0219)和 BCL-2(P = 0.0338)的含量增加。最后,通过质谱对EVs蛋白质含量的研究发现,EVs携带了多种参与已知致癌途径的蛋白质,而对是否使用NLCs EVs处理的CLL-B细胞进行的RNAseq分析则显示了多种不同的表达基因。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Cancer gene therapy
医学-生物工程与应用微生物
CiteScore
10.20
自引率
0.00%
发文量
150
审稿时长
4-8 weeks
期刊介绍:
Cancer Gene Therapy is the essential gene and cellular therapy resource for cancer researchers and clinicians, keeping readers up to date with the latest developments in gene and cellular therapies for cancer. The journal publishes original laboratory and clinical research papers, case reports and review articles. Publication topics include RNAi approaches, drug resistance, hematopoietic progenitor cell gene transfer, cancer stem cells, cellular therapies, homologous recombination, ribozyme technology, antisense technology, tumor immunotherapy and tumor suppressors, translational research, cancer therapy, gene delivery systems (viral and non-viral), anti-gene therapy (antisense, siRNA & ribozymes), apoptosis; mechanisms and therapies, vaccine development, immunology and immunotherapy, DNA synthesis and repair.
Cancer Gene Therapy publishes the results of laboratory investigations, preclinical studies, and clinical trials in the field of gene transfer/gene therapy and cellular therapies as applied to cancer research. Types of articles published include original research articles; case reports; brief communications; review articles in the main fields of drug resistance/sensitivity, gene therapy, cellular therapy, tumor suppressor and anti-oncogene therapy, cytokine/tumor immunotherapy, etc.; industry perspectives; and letters to the editor.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


