Examining Cesarean Among Individuals of Advanced Maternal Age in Nurse-Midwifery Care
Abstract
Introduction
Cesarean rates are rising, especially for individuals of advanced maternal age (AMA), defined as aged 35 or older. The Robson 10-Group Classification System (TGCS) facilitates assessment and comparison of cesarean rates among individuals in different settings. In midwifery-led care, in which pregnant people are typically healthier and seek a vaginal birth, it is unknown whether individuals of AMA have different antecedents leading to cesarean compared with younger counterparts. This study aimed to examine antecedents contributing to cesarean using Robson TGCS for individuals across age groups in midwifery care.
Methods
This study was a secondary analysis of 2 cohort data sets from Oregon Health & Science University (OHSU) and University of Michigan Health Systems (UMHS) hospitals. The samples were individuals in midwifery-led care birthing at either OHSU from 2012 to 2019 or UMHS from 2007 to 2019.
Results
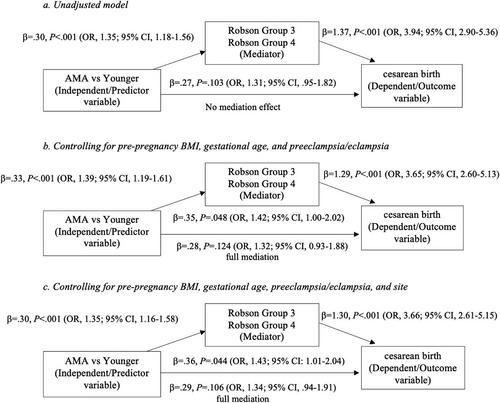
A total of 11,951 individuals were studied. Overall cesarean rates were low; however, the rate for individuals of AMA was higher than the rate of their younger counterparts (18.30% vs 15.10%). The Robson groups were similar; however, the primary contributor among AMA individuals was group 5 (multiparous with previous cesarean), followed by group 2 [nulliparous with labor induced or prelabor cesarean], and group 1 [nulliparous with spontaneous labor]. In contrast, the primary contributors for younger individuals were groups 1, 2, and 5, respectively. In addition, prelabor cesarean and induced labor partly mediated the relationship between AMA and cesarean among nulliparous individuals, whereas prelabor cesarean was the key contributor to cesarean among multiparous people.
Discussion
The cesarean rate in midwifery-led care was low. Using Robson TGCS provided additional insight into the antecedents to cesarean, rather than viewing cesarean as a single outcome. Future studies should continue to use Robson TGCS and investigate antecedents to cesarean, including factors influencing successful vaginal birth after cesarean in individuals of AMA.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


