Patient-reported outcomes and treatment adherence in type 2 diabetes using natural language processing: Wave 8 of the Observational International Diabetes Management Practices Study
Abstract
Aims/Introduction
We analyzed patient-reported outcomes of people with type 2 diabetes to better understand perceptions and experiences contributing to treatment adherence.
Materials and Methods
In the ongoing International Diabetes Management Practices Study, we collected patient-reported outcomes data from structured questionnaires (chronic treatment acceptance questionnaire and Diabetes Self-Management Questionnaire) and free-text answers to open-ended questions to assess perceptions of treatment value and side-effects, as well as barriers to, and enablers for, adherence and self-management. Free-text answers were analyzed by natural language processing.
Results
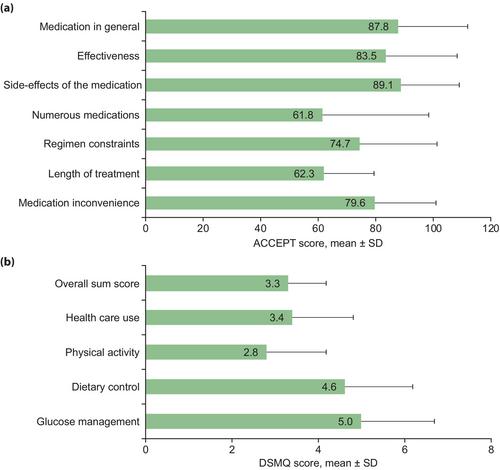
In 2018–2020, we recruited 2,475 patients with type 2 diabetes (43.3% insulin-treated, glycated hemoglobin (HbA1c) 8.0 ± 1.8%; 30.9% with HbA1c <7%) from 13 countries across Africa, the Middle East, Europe, Latin America and Asia. Mean ± standard deviation scores of chronic treatment acceptance questionnaire (acceptance of medication, rated out of 100) and Diabetes Self-Management Questionnaire (self-management, rated out of 10) were 87.8 ± 24.5 and 3.3 ± 0.9, respectively. Based on free-text analysis and coded responses, one in three patients reported treatment non-adherence. Overall, although most patients accepted treatment values and side-effects, self-management was suboptimal. Treatment duration, regimen complexity and disruption of daily routines were major barriers to adherence, whereas habit formation was a key enabler. Treatment-adherent patients were older (60 ± 11.6 vs 55 ± 11.7 years, P < 0.001), and more likely to have longer disease duration (12 ± 8.6 vs 10 ± 7.7 years, P < 0.001), exposure to diabetes education (73.1% vs 67.8%, P < 0.05), lower HbA1c (7.9 ± 1.8% vs 8.3 ± 1.9%, P < 0.001) and attainment of HbA1c <7% (29.7% vs 23.3%, P < 0.01).
Conclusions
Patient perceptions/experiences influence treatment adherence and self-management. Patient-centered education and support programs that consider patient-reported outcomes aimed at promoting empowerment and developing new routines might improve glycemic control.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


