Excess prevalence of preexisting chronic conditions in older adults with incident epilepsy
Abstract
Objective
Prior studies have examined chronic conditions in older adults with prevalent epilepsy, but rarely among those with incident epilepsy. Identifying the chronic conditions with which older adults present at epilepsy incidence assists with the evaluation of disease burden in this patient population and informs coordinated care development. The aim of this study was to identify preexisting chronic conditions with excess prevalence in older adults with incident epilepsy compared to those without.
Methods
Using a random sample of 4 999 999 fee-for-service Medicare beneficiaries aged >65 years, we conducted a retrospective cohort study of epilepsy incidence in 2019. Non-Hispanic Black and Hispanic beneficiaries were oversampled. We identified preexisting chronic conditions from the 2016–2018 Medicare Beneficiary Summary Files and compared chronic condition prevalence between Medicare beneficiaries with and without incident epilepsy in 2019. We characterized variations in preexisting excess chronic condition prevalence by age, sex, and race/ethnicity, adjusting for the racial/ethnic oversampling.
Results
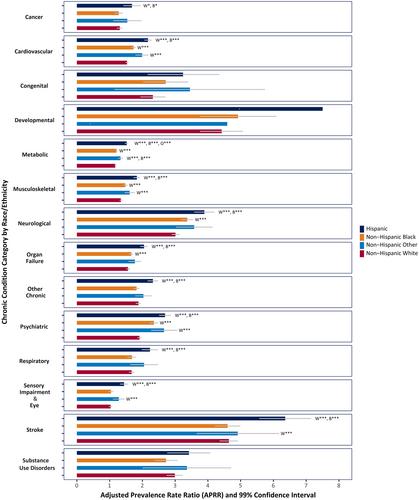
We observed excess prevalence of most preexisting chronic conditions in beneficiaries with incident epilepsy (n = 20 545, weighted n = 19 631). For stroke, for example, the adjusted prevalence rate ratio (APRR) was 4.82 (99% CI:4.60, 5.04), meaning that, compared to those without epilepsy, beneficiaries with incident epilepsy in 2019 had 4.82 times the stroke prevalence. Similarly, beneficiaries with incident epilepsy had a higher prevalence rate for preexisting neurological conditions (APRR = 3.17, 99% CI = 3.08–3.27), substance use disorders (APRR = 3.00, 99% CI = 2.81–3.19), and psychiatric disorders (APRR = 1.98, 99% CI = 1.94–2.01). For most documented chronic conditions, excess prevalence among beneficiaries with incident epilepsy in 2019 was larger for younger age groups compared to older age groups, and for Hispanic beneficiaries compared to both non-Hispanic White and non-Hispanic Black beneficiaries.
Significance
Compared to epilepsy-free Medicare beneficiaries, those with incident epilepsy in 2019 had a higher prevalence of most preexisting chronic conditions. Our findings highlight the importance of health promotion and prevention, multidisciplinary care, and elucidating shared pathophysiology to identify opportunities for prevention.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


