Cost-Effectiveness and Budget Impact Analysis of the Implementation of Differentiated Service Delivery Models for HIV Treatment in Mozambique: a Modelling Study
Abstract
Introduction
In 2018, the Mozambique Ministry of Health launched guidelines for implementing differentiated service delivery models (DSDMs) to optimize HIV service delivery, improve retention in care, and ultimately reduce HIV-associated mortality. The models were fast-track, 3-month antiretrovirals dispensing, community antiretroviral therapy groups, adherence clubs, family approach and three one-stop shop models: adolescent-friendly health services, maternal and child health, and tuberculosis. We conducted a cost-effectiveness analysis and budget impact analysis to compare these models to conventional services.
Methods
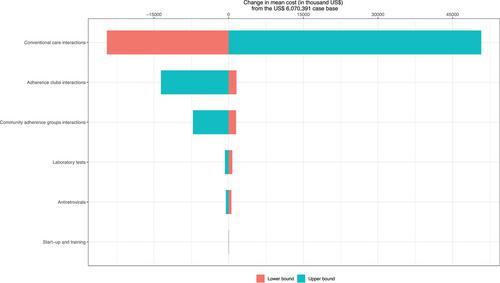
We constructed a decision tree model based on the percentage of enrolment in each model and the probability of the outcome (12-month retention in treatment) for each year of the study period—three for the cost-effectiveness analysis (2019–2021) and three for the budget impact analysis (2022–2024). Costs for these analyses were primarily estimated per client-year from the health system perspective. A secondary cost-effectiveness analysis was conducted from the societal perspective. Budget impact analysis costs included antiretrovirals, laboratory tests and service provision interactions. Cost-effectiveness analysis additionally included start-up, training and clients’ opportunity costs. Effectiveness was estimated using an uncontrolled interrupted time series analysis comparing the outcome before and after the implementation of the differentiated models. A one-way sensitivity analysis was conducted to identify drivers of uncertainty.
Results
After implementation of the DSDMs, there was a mean increase of 14.9 percentage points (95% CI: 12.2, 17.8) in 12-month retention, from 47.6% (95% CI, 44.9–50.2) to 62.5% (95% CI, 60.9–64.1). The mean cost difference comparing DSDMs and conventional care was US$ –6 million (173,391,277 vs. 179,461,668) and –32.5 million (394,705,618 vs. 433,232,289) from the health system and the societal perspective, respectively. Therefore, DSDMs dominated conventional care. Results were most sensitive to conventional care interaction costs in the one-way sensitivity analysis. For a population of 1.5 million, the base-case 3-year financial costs associated with the DSDMs was US$550 million, compared with US$564 million for conventional care.
Conclusions
DSDMs were less expensive and more effective in retaining clients 12 months after antiretroviral therapy initiation and were estimated to save approximately US$14 million for the health system from 2022 to 2024.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


