Midwifery continuity of care for women with perinatal mental health conditions: A cohort study from Australia
Abstract
Background
Perinatal mental health (PMH) conditions are associated with adverse outcomes such as maternal suicide, preterm birth and longer-term childhood sequelae. Midwifery continuity of care (one midwife or a small group of midwives) has demonstrated benefits for women and newborns, including a reduction in preterm birth and improvements in maternal anxiety/worry and depression.
Aim
To determine if midwifery care provided through a Midwifery Group Caseload Practice model is associated with improved perinatal outcomes for women who have anxiety and depression and/or other perinatal mental health conditions. An EPDS ≥ 13, and/or answered the thought of harming myself has occurred to me and/or women who self-reported a history compared to standard models of care (mixed midwife/obstetric fragmented care).
Methods
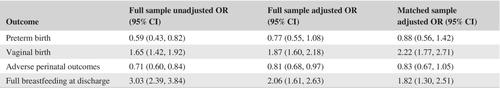
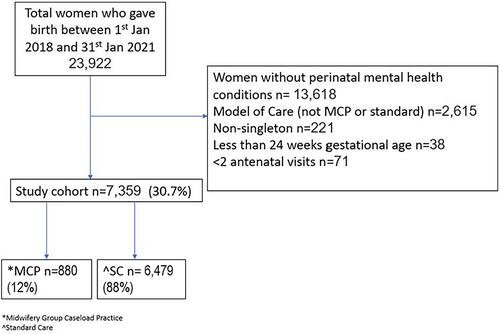
A retrospective cohort study using data routinely collected via an electronic database between 1 January 2018 31st of January 2021. The population were women with current/history of PMH, who received Midwifery Caseload Group Practice (MCP), or standard care (SC). Data were analysed using descriptive statistics for maternal characteristics and logistic regression for birth outcomes. One-to-one matching of the MCP group with the SC group was based on propensity scores.
Results
7,359 births were included MCP 12% and SC 88%. Anxiety was the most common PMH with the same proportion affected in MCP and SC. Adjusted odds of preterm birth and adverse perinatal outcomes were lower in the MCP group than the SC group (aOR (95%CI): 0.77 (0.55, 1.08) and 0.81 (0.68, 0.97), respectively) and higher for vaginal birth and full breastfeeding (aOR (95% CI): 1.87 (1.60, 2.18) and 2.06 (1.61, 2.63), respectively). In the matched sample the estimate of a relationship between MCP and preterm birth (aOR (95% CI): 0.88 (0.56, 1.42), adverse perinatal outcomes (aOR (95% CI): 0.83 (0.67, 1.05)) and breastfeeding at discharge (aOR (95% CI): 1.82 (1.30, 2.51)), stronger for vaginal birth (aOR (95% CI): 2.22 (1.77, 2.71)).
Conclusion
This study supports positive associations between MCP and breastfeeding and vaginal birth. MCP was also associated with lower risk of adverse perinatal outcomes, though in the matched sample with a smaller sample size, the confidence interval included 1. The direction of the association MCP and preterm birth was negative (protective). However, in the matched sample analysis, the confidence interval was wide, and the finding was also consistent with no benefit from MCP. Randomised controlled trials are required to answer questions around preterm birth and adverse perinatal outcomes and further research is being planned.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


