Differing contributions of the gut microbiota to the blood pressure lowering effects induced by first-line antihypertensive drugs
Abstract
Background and Purpose
This study analyses whether first-line antihypertensive drugs ameliorate the dysbiosis state in hypertension, and to test if this modification contributes to their blood pressure (BP) lowering properties in a genetic model of neurogenic hypertension.
Experimental Approach
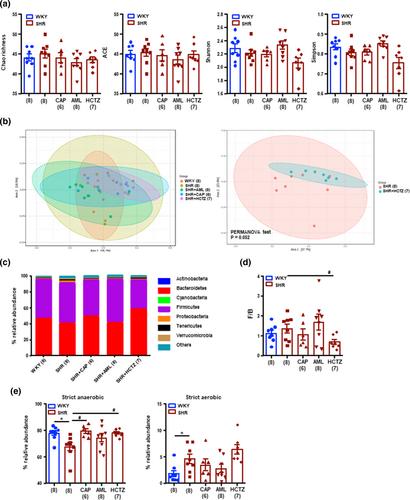
Twenty-week-old male Wistar Kyoto rats (WKY) and spontaneously hypertensive rats (SHR) were untreated or treated with captopril, amlodipine or hydrochlorothiazide. A faecal microbiota transplantation (FMT) experiment was also performed by gavage of faecal content from donor SHR-treated groups to SHR recipients for 3 weeks.
Key results
Faeces from SHR showed gut dysbiosis, characterized by lower acetate- and higher lactate-producing bacteria and lower strict anaerobic bacteria. All three drugs increased the anaerobic bacteria proportion, captopril and amlodipine restored the proportion of acetate-producing bacterial populations to WKY levels, whereas hydrochlorothiazide decreased butyrate-producing bacteria. Captopril and amlodipine decreased gut pathology and permeability and attenuated sympathetic drive in the gut. Both drugs decreased neuroinflammation and oxidative stress in the hypothalamic paraventricular nuclei. Hydrochlorothiazide was unable to reduce neuroinflammation, gut sympathetic tone and gut integrity. FMT from SHR-amlodipine to SHR decreased BP, ameliorated aortic endothelium-dependent relaxation to acetylcholine, lowered NADPH oxidase activity, aortic Th17 infiltration and reduced neuroinflammation, whereas FMT from SHR-hydrochlorothiazide did not have these effects.
Conclusions and Implications
First-line antihypertensive drugs induced different modifications of gut integrity and gut dysbiosis in SHR, which result in no contribution of microbiota in the BP lowering effects of hydrochlorothiazide, whereas the vasculo-protective effect induced by amlodipine involves gut microbiota reshaping and gut-immune system communication.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


