Association of health confidence with hospital length of stay and readmission
Abstract
Background
Length of stay (LOS) is an important measure of hospital quality and may be impacted by patient participation. However, concepts of patient participation, like health confidence, have received little examination in hospitalized patients' LOS, especially in diverse populations.
Objective
To determine if the Health Confidence Score (HCS) is associated with hospital LOS and readmission in a socioeconomically diverse population.
Designs, Settings, and Participants
We conducted a prospective cohort study in 2022 of adult general medicine patients at an academic hospital in Chicago, Illinois.
Intervention
None.
Main Outcome and Measures
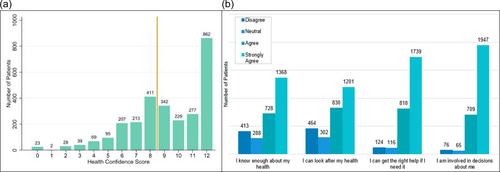
Patient-reported responses to the HCS (scored 0 [lowest health confidence] to ‒12 [highest health confidence]), as well as demographic, socioeconomic, and clinical questions, were collected. Primary outcome was LOS and secondary outcomes were 30- and 90-day readmission.
Results
Among 2797 socioeconomically diverse patients who completed the survey (response rate 28.5%), there was an average HCS of 9.19 (SD 2.68, range 0–12). Using linear regression, patients with high HCS (HCS ≥ 9) had a 1.53-day lower LOS (p < .01, 95% confidence interval [CI] [–2.11, –0.95]) than patients with a low HCS (HCS < 9). This association remained when examining individual HCS questions and controlling for covariates. In logistic regression, HCS was not significantly associated with readmission, but the question “I am involved in decisions about me” (adjusted model: odds ratio 0.83; 95% CI [0.71, 0.96]; p = .01) was associated with 90-day readmission.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


