Impact of diabetes on the prognosis of patients with oral and oropharyngeal cancer: A meta-analysis
Abstract
Aims/Introduction
Diabetes has been related to an increased risk of oral cancer. Nevertheless, the impact of diabetes on the outcome of individuals with oral and oropharyngeal cancer is not clear. In this study, a meta-analysis was carried out to assess the link between diabetes and the survival of individuals with oral and oropharyngeal cancer.
Materials and Methods
Relevant cohort studies for the meta-analysis objective were obtained through searching electronic databases, such as PubMed, Web of Science and Embase. The data were combined using a random effects model that accounted for differences between studies.
Results
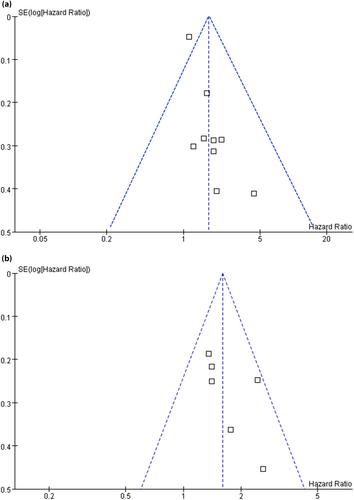
A total of 10 cohorts involving 21,871 patients with oral and oropharyngeal cancer were included. Pooled results suggest that compared with those with normoglycemia, oral and oropharyngeal cancer patients with diabetes were associated with a poor overall survival (hazard ratio 1.69, 95% confidence interval 1.29–2.22, P < 0.001; I2 = 69%). Subgroup analysis suggested a stronger association between diabetes and poor overall survival in patients aged ≥52 years as compared with those aged <52 years (hazard ratio 2.08 vs 1.34, P = 0.03). Other study characteristics, such as study country, tumor stage or follow-up duration, did not seem to significantly affect the association (P for subgroup difference all >0.05). In addition, diabetes was also associated with a poor progression-free survival of patients with oral and oropharyngeal cancer (hazard ratio 1.61, 95% confidence interval 1.30–1.99, P < 0.001; I2 = 9%).
Conclusions
Patients with oral and oropharyngeal cancer might have a poor survival if they have pre-existing diabetes.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


