Predictors of prolonged hospital stay after segmentectomy
IF 4.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-02-01
DOI:10.1016/j.jtcvs.2024.04.021
引用次数: 0
Abstract
Objective
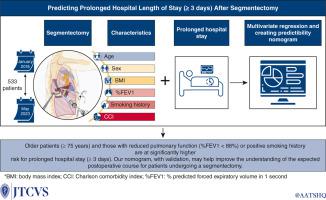
Segmentectomy is becoming the standard of care for small, peripheral non–small cell lung cancer. To improve perioperative management in this population, this study aims to identify factors influencing hospital length of stay after segmentectomy.
Methods
Patients who underwent segmentectomy for any indication between January 2018 and May 2023 were identified using a prospectively maintained institutional database. Multivariable logistic regression models were used to estimate associations between clinical features and prolonged (≥3 days) hospital stay. A nomogram was designed to understand better and possibly calculate the individual risk of prolonged hospital stays.
Results
In total, 533 cases were included; 337 (63%) were female. Median age was 66 years (interquartile range [IQR], 63-75). The median size of resected lesions was 1.6 cm (IQR, 1.3-2.1 cm). Median hospital stay was 3 days (IQR, 2-4 days). Major adverse events occurred in 31 (5.8%) cases. The 30-day readmission rate was 5.8% (n = 31). There was no 30-day mortality; 90-day mortality was <1%. Patients older than 75 years (odds ratio [OR], 2.01, 95% confidence interval [CI], 1.15-3.57, P = .02), those with forced expiratory volume in 1 second <88% predicted (OR, 1.99; 95% CI, 1.38-2.89, P < .001), or positive smoking history (OR, 1.72; 95% CI, 1.15-2.60, P = .01) were more likely to have prolonged hospital stays after segmentectomy. A nomogram accounting for age, sex, forced expiratory volume in 1 second, body mass index, smoking history, and comorbidities was created to predict the probability of prolonged hospital stay with an area under the receiver operating characteristic curve of 0.66.
Conclusions
Older patients, those with reduced pulmonary function, and current and past smokers have elevated risk for prolonged hospital stays after segmentectomy. Validation of our nomogram could improve perioperative risk stratification in patients who undergo segmentectomy.

节段切除术后住院时间延长的预测因素
目的:肺段切除术正在成为治疗周围非小细胞肺癌的标准方法。为了改善这一人群的围手术期管理,本研究旨在确定影响肺段切除术后住院时间的因素:使用前瞻性维护的机构数据库,对2018年1月至2023年5月期间因任何适应症接受肺段切除术的患者进行识别。使用多变量逻辑回归模型估计临床特征与住院时间延长(≥ 3 天)之间的关系。设计了一个提名图,以更好地了解并计算个人住院时间延长的风险:共纳入 533 例病例,其中 337 例(63%)为女性。中位年龄为 66 岁(IQR:63-75)。切除病灶的中位尺寸为 1.6 厘米(IQR:1.3-2.1)。住院时间中位数为 3 天(IQR:2-4)。31例(5.8%)发生了重大不良事件。30天再入院率为5.8%(n=31)。无 30 天死亡病例;90 天死亡病例为结论:老年患者、肺功能减退者、当前和过去吸烟者在肺段切除术后住院时间延长的风险较高。对我们的提名图进行验证可改善肺段切除术患者围手术期的风险分层。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


