Risk factors of bleeding during rectal cancer surgery in obese patients in Japan
Abstract
Background
According to several clinical trials for patients with rectal cancer, laparoscopic surgery significantly reduces intraoperative complications and bleeding compared with laparotomy and demonstrated comparable long-term results. However, obesity is considered one of the risk factors for increased surgical difficulty, including complication rate, prolonged operation time, and bleeding.
Methods
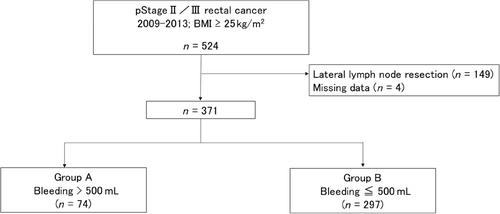
Patients with clinical pathological stage II/III rectal cancer and a body mass index of ≥25 kg/m2 who underwent laparotomy or laparoscopic surgery between January 2009 and December 2013 at 51 institutions participating in the Japan Society of Laparoscopic Colorectal Surgery were included. These patients were divided into major bleeding (>500 mL) group and minor bleeding (≤500 mL) group. The risk factors of major bleeding were evaluated by univariate and multivariate analyses.
Results
This study included 517 patients, of which 74 (19.9%) experienced major bleeding. Patient characteristics did not significantly differ between the two groups. The major bleeding group had a longer operative time (p < 0.001) and a larger tumor size than the minor bleeding group (p = 0.011). In the univariate analysis, age >65 years, laparotomy, operative time >300 min, and multivisceral resection were significantly associated with intraoperative massive bleeding. In the multivariate analysis, age >65 years (odds ratio [OR], 2.29; 95% confidence interval [CI], 1.13–4.82), laparotomy (OR, 20.82; 95% CI, 11.56–39.75), operative time >300 min (OR, 5.39; 95% CI, 1.67–132), and multivisceral resection (OR, 10.72; 95% CI, 2.47–64.0) showed to be risk factors for massive bleeding.
Conclusion
Age >65 years, laparotomy, operative time >300 min, and multivisceral resection were risk factors for massive bleeding during rectal cancer surgery in patients with obesity.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


