Characterization and modulation of the pro-inflammatory effects of immune cells in the canine intervertebral disk
Abstract
Background
Intervertebral disk (IVD) degeneration affects both humans and canines and is a major cause of low back pain (LBP). Mast cell (MC) and macrophage (MØ) infiltration has been identified in the pathogenesis of IVD degeneration (IVDD) in the human and rodent model but remains understudied in the canine. MC degranulation in the IVD leads to a pro-inflammatory cascade and activates protease activated receptor 2 (PAR2) on IVD cells. The objectives of the present study are to: (1) highlight the pathophysiological changes observed in the degenerate canine IVD, (2) further characterize the inflammatory effect of MCs co-cultured with canine nucleus pulposus (NP) cells, (3) evaluate the effect of construct stiffness on NP and MCs, and (4) identify potential therapeutics to mitigate pathologic changes in the IVD microenvironment.
Methods
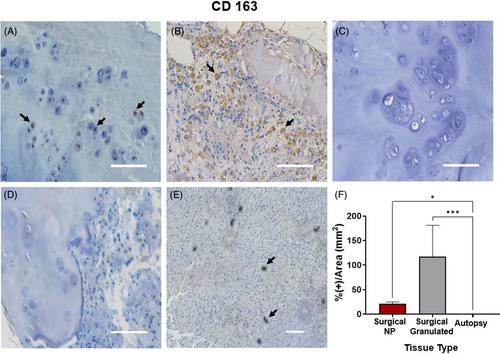
Canine IVD tissue was isolated from healthy autopsy research dogs (beagle) and pet dogs undergoing laminectomy for IVD herniation. Morphology, protein content, and inflammatory markers were assessed. NP cells isolated from healthy autopsy (Mongrel hounds) tissue were co-cultured with canine MCs within agarose constructs and treated with cromolyn sodium (CS) and PAR2 antagonist (PAR2A). Gene expression, sulfated glycosaminoglycan content, and stiffness of constructs were assessed.
Results
CD 31+ blood vessels, mast cell tryptase, and macrophage CD 163+ were increased in the degenerate surgical canine tissue compared to healthy autopsy. Pro-inflammatory genes were upregulated when canine NP cells were co-cultured with MCs and the stiffer microenvironment enhanced these effects. Treatment with CS and PAR2 inhibitors mediated key pro-inflammatory markers in canine NP cells.
Conclusion
There is increased MC, MØs, and vascular ingrowth in the degenerate canine IVD tissue, similar to observations in the clinical population with IVDD and LBP. MCs co-cultured with canine NP cells drive inflammation, and CS and PAR2A are potential therapeutics that may mitigate the pathophysiology of IVDD in vitro.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


