Use of a dosimetry-based RAI protocol for treatment of benign hyperthyroidism optimises response while minimising exposure to ionising radiation
Abstract
Background
The optimal treatment strategy for radioiodine (RAI) treatment protocols for benign hyperthyroidism remains elusive. Although individualised activities are recommended in European Law, many centres continue to provide fixed activities. Our institution implemented a dosimetry protocol in 2016 following years of fixed dosing which facilitates the calculation of individualised activities based on thyroid volume and radioiodine uptake.
Methods
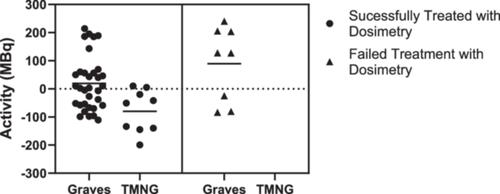
This was a retrospective study comparing success rates using a dosimetry protocol targeting an absorbed dose of 150 Gy for Graves’ disease (GD) and 125 Gy for Toxic Multinodular Goiter (TMNG) with fixed dosing (200MBq for GD and 400MBq for TMNG) among 204 patients with hyperthyroidism. Success was defined as a non-hyperthyroid state at 1 year for both disease states. Results were analysed for disease specific or patient specific modulators of response.
Results
This study included 204 patients; 74% (n = 151) received fixed activities and 26% (n = 53) of activities administered were calculated using dosimetry. A dosimetry-based protocol was successful in 80.5% of patients with GD and 100% of patients with TMNG. Differences in success rates and median activity administered between the fixed (204Mbq) and dosimetry (246MBq) cohort were not statistically significant (p = .64) however 44% of patients with GD and 70% of patients with TMNG received lower activities following treatment with dosimetry as opposed to fixed activities. Use of dosimetry resulted in successful treatment and reduced RAI exposure for 36% of patients with GD, 70% of patients with TMNG, and 44% of patients overall.
Conclusion
This retrospective clinical study demonstrated that treatment with a dosimetry-based protocol for TMNG and GD achieved comparable success rates to fixed protocols while reducing RAI exposure for over a third of patients with GD and most patients with TMNG. This study also highlighted that RAI can successfully treat hyperthyroidism for some patients with activities lower than commonplace in clinical practise. No patient or disease specific modulators of treatment response were established in this study; however, the data supports a future prospective trial which further scrutinises the individual patient factors governing treatment response to RAI.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


