Improving accuracy of outcome prediction for infants born extremely preterm using a digital tool: Translating ‘NIC-PREDICT’ into clinical practice, the first steps
Abstract
Background
Many clinicians overestimate mortality and disability rates in infants born extremely preterm. We developed a digital tool (‘NIC-PREDICT’) that predicts infant mortality and survival with and without major disability in infants born 23–27 weeks' gestation.
Aims
To determine if clinicians could use NIC-PREDICT accurately, and if their perceptions of infant outcomes improved after its release in 2021.
Materials and Methods
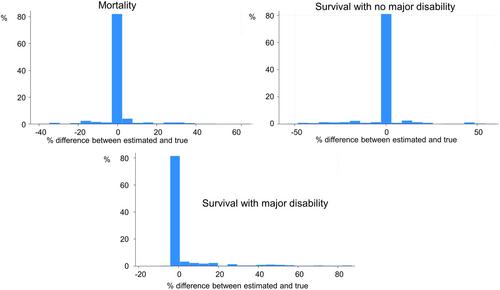
Midwives, nurses, obstetricians, neonatologists and paediatricians working in tertiary and non-tertiary hospitals in Victoria were asked to use NIC-PREDICT to estimate three mutually exclusive outcomes: (i) mortality; (ii) survival free of major disability; and (iii) survival with major disability for six different scenarios where a liveborn infant was offered survival-focused care after birth. The proportions who completed the survey (responded to all six scenarios) and the proportions able to provide 100% accurate results for all scenarios were determined. Estimates of the three outcomes were compared with true rates.
Results
A total of 85 clinicians responded: 70 (82%) completed the survey, with an overall accuracy of 76%. Overall, predictions of mortality were accurate (mean difference from true value 0.7% (95% confidence interval (CI) −0.7, 2.1) P = 0.33), as were predictions of survival without major disability (mean difference − 0.7 (95% CI –3.0, 1.7) P = 0.58). However, survival with major disability was overestimated by 4.9% ((95% CI 1.7, 8.0) P = 0.003).
Conclusions
Most perinatal clinicians who responded used NIC-PREDICT correctly to estimate expected outcomes in infants born extremely preterm who are offered intensive care. Undue pessimism about survival with major disability remains an ongoing concern.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


