Evaluation of single maintenance and reliever therapy (SMART) prescribing of budesonide-formoterol for asthma after a clinical pharmacist-led initiative
Abstract
Introduction
Single maintenance and reliever therapy (SMART) with a combination inhaled corticosteroid-formoterol inhaler is the preferred asthma treatment by the Global Initiative for Asthma and the National Asthma Education and Prevention Program guidelines. These recommendations have been slow to be implemented routinely into clinical practice.
Methods
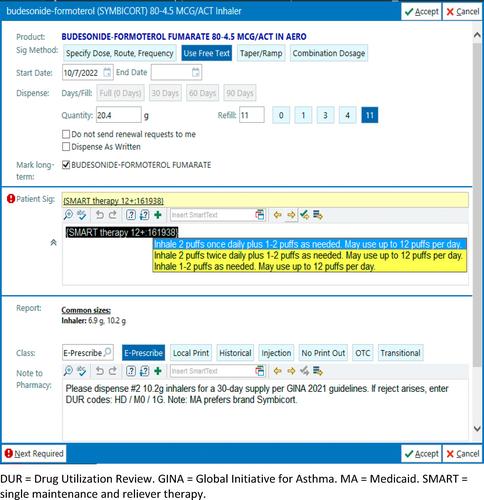
This was an observational cohort study conducted in a family medicine residency program clinic. A clinical pharmacist-led initiative to implement SMART, which included provider education and the development of clinical tools to facilitate SMART prescribing, was assessed. Year 1 (Y1; pre-intervention) and year 2 (Y2; post-intervention) were compared.
Outcomes
The primary outcome was to evaluate the impact of this initiative on the frequency of SMART (budesonide-formoterol without albuterol) prescribing. Prescription frequencies for albuterol and budesonide-formoterol were also compared separately. Secondary outcomes were Asthma Control Test (ACT) scores and prescribing frequencies among faculty and resident physicians.
Results
The total number of eligible patients in the clinic population was 807, and 459 of these patients met the inclusion criteria. There were more females than males, and the mean age was 39. About 24% had a language preference other than English and 22% required an interpreter. The percentage of patients who were prescribed SMART significantly increased from 0.44% to 11.5% (p < 0.001). Budesonide-formoterol prescriptions increased from 7.4% to 34.6% (p < 0.001). Albuterol metered-dose inhaler prescriptions decreased from 79.7% to 66.2% (p < 0.001). Prescribing patterns were similar for patients of faculty physicians (n = 258) and resident physicians (n = 196). Only 164 (35.7%) patients had an ACT score in Y1 and Y2, and the mean ACT score was not significantly different between Y1 and Y2 (p = 0.973).
Conclusion
A clinical pharmacist-led SMART asthma prescribing initiative was associated with a significant increase in SMART prescribing, a significant increase in budesonide-formoterol prescribing, and a significant decrease in albuterol prescribing.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


