Exploring experiences of living with removable dentures—A scoping review of qualitative literature
Abstract
Objective
Examine the literature on the experiences of living with removable dentures (complete or partial) to identify any gaps and provide a map for future research.
Background
Increasing proportions of society are living partially dentate with some form of restoration, including removable dentures. Previous studies have reported on the location, materials and usage of these prostheses, along with effects on oral-health-related quality of life (OHRQoL). However, less is known about experiences with removable dentures from a patient-centred perspective.
Methods
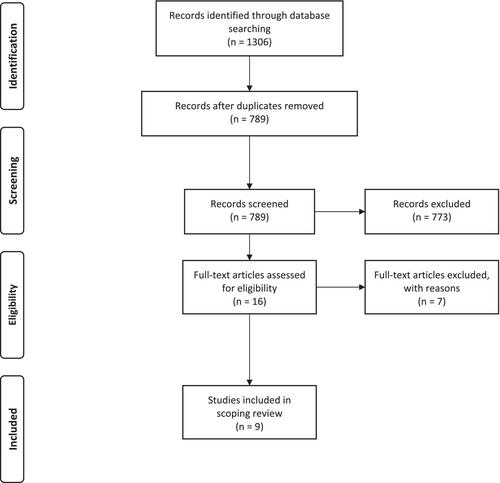
A scoping review of the qualitative literature was undertaken using the framework of Arksey and O'Malley, updated by Levac et al. Literature searches were carried out using Medline and Web of Science. Papers were screened by title and abstract using inclusion and exclusion criteria. Remaining papers were read in full and excluded if they did not meet the required criteria. Nine papers were included in the final review.
Findings
Key themes from these papers were: impact of tooth loss and living without teeth, and its impacts in relation to social position, appearance, confidence and function (chewing and speaking); social norms and tooth loss, including attitudes to tooth retention and treatment costs, and changes in intergenerational norms towards dentures; expectations of treatment, including patients being more involved in decision making, viewing the denture as a “gift” and dentures helping to achieve “an ideal”; living with a removable denture (complete or partial), including patient preparedness for a denture, adaptation and impacts on activities and participation; and the dentist-patient relationship, including issues with information and communication, and differing priorities between patients and dentists.
Conclusion
Little qualitative research exists on experiences of living with a removable denture. Existing literature demonstrates the importance of dispersed activities in differing social, spatial and temporal contexts when wearing removable dentures. Focusing on processes of positive adaptation to dentures and OHRQoL, rather than deficits, is also required to fully understand patients' experiences. Additionally, more complex technological advances may not always be in the best interest of every patient.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


