Point-of-care ultrasound is a useful adjunct tool to a clinician's assessment in the evaluation of severe hyponatraemia
Abstract
Introduction
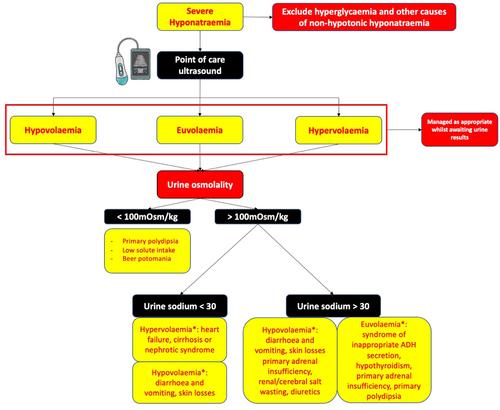
Hyponatraemia is the most common electrolyte disorder in inpatients resulting mainly from an imbalance in water homeostasis. Intravascular fluid status assessment is pivotal but is often challenging given multimorbidity, polypharmacy and diuretics use. We evaluated the utility of point-of-care ultrasound (POCUS) as an adjunct tool to standard practice for fluid assessment in severe hyponatraemia patients.
Methods
Patients presenting with severe hyponatremia (Serum Sodium [Na] < 120 mmol/L; Normal range: 135−145 mol/L), managed by standard care were included. Hyponatraemia biochemistry work-up and POCUS examination were undertaken. Both clinician and POCUS independently assigned one of the three fluid status groups of hypovolaemia, hypervolaemia or euvolaemia. The final diagnosis of three fluid status groups at admission was made at the time of discharge by retrospective case review. Clinician's (standard of care) and POCUS fluid assessments were compared to that of the final diagnosis at the time of discharge.
Results
n = 19 patients were included. Median Na on admission was 113 mmol/L (109-116), improved to 129 ± 3 mmol/L on discharge. POCUS showed the higher degree of agreement with the final diagnosis (84%; n = 16/19), followed by the clinician (63%; n = 12/19). A trend towards higher accuracy of POCUS compared to clinician assessment of fluid status was noted (84% vs. 63%, p = 0.1611). Biochemistry was unreliable in 58% (n = 11/19) likely due to renal failure, polypharmacy or diuretic use. Inappropriate emergency fluid management was undertaken in 37% (n = 7/19) of cases based on initial clinician assessment. Thirst symptom correlated to hypovolaemia in 80% (4/5) cases.
Conclusion
As subjective clinical and biochemistry assessments of fluid status are often unreliable due to co-morbidities and concurrent use of medications, POCUS can be a rapid objective diagnostic tool to assess fluid status in patients with severe hyponatraemia, to guide accurate emergency fluid management.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


