Comparing 3-year survival and readmissions between HeartMate 3 and heart transplant as primary treatment for advanced heart failure
IF 4.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-01-01
DOI:10.1016/j.jtcvs.2023.12.019
引用次数: 0
Abstract
Objective
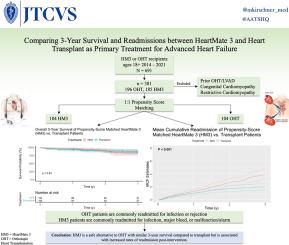
To compare 3-year survival and readmissions of patients who received the HeartMate 3 (HM3) left ventricular assist device (LVAD) or underwent orthotopic heart transplantation (OHT) as primary treatment for advanced heart failure.
Methods
We retrospectively analyzed 381 adult patients who received an HM3 LVAD or were listed for OHT between January 2014 and March 2021 at our center. To minimize crossover bias, OHT recipients with a prior LVAD were excluded, and HM3 patients were censored at the time of transplant. Cohorts were propensity score–matched to reduce confounding variables. The primary outcome was 3-year survival, and the secondary outcome was mean cumulative all-cause unplanned readmission.
Results
The study population comprised 185 HM3 patients (49%) and 196 OHT patients (51%), with 104 propensity score–matched patients in each group. After propensity score matching, there was no statistical difference in 3-year survival (83.7% for HM3 vs 87.0% for OHT; P = .91; relative risk [RR], 1.00; 95% confidence interval [CI], 0.45-2.20). In the unmatched cohorts, patients age 18 to 49 years had comparable survival with HM3 and OHT (96.9% vs 95.9%; N = 91; P = 1.00; RR, 0.92; 95% CI, 0.09-9.78). Patients age 50+ years had slightly inferior survival with HM3 (75.0% vs 83.9%; N = 290; P = .60; RR, 1.51; 95% CI, 0.85-2.68). The mean number of readmissions at 3 years was higher in the HM3 group (3.89 vs 2.05; P < .001).
Conclusions
This exploratory analysis suggests that for similar patients, HM3 may provide comparable 3-year survival to OHT as a primary treatment for heart failure but may result in more readmissions.
比较作为晚期心力衰竭主要治疗方法的 HeartMate 3 和心脏移植手术的 3 年生存率和再住院率
目标我们的目标是比较接受 HeartMate 3(HM3)左心室辅助装置(LVAD)或正位心脏移植(OHT)作为晚期心衰主要治疗方法的患者的 3 年生存率和再住院率。方法我们回顾性分析了 2014 年 1 月至 2021 年 3 月期间在本中心接受 HM3 LVAD 或列入 OHT 的 381 名成年患者。为了尽量减少交叉偏倚,我们排除了曾接受过 LVAD 的 OHT 患者,并在移植时对 HM3 患者进行了剔除。队列采用倾向评分匹配(PSM),以减少混杂变量。主要结果是 3 年存活率。结果各组包括 185 名(49%)HM3 患者和 196 名(51%)OHT 患者,每组有 104 名 PSM 患者。PSM 后,3 年生存率无统计学差异(HM3 83.7% 对 OHT 87.0%,P = 0.91;RR = 1.00,95% CI = 0.45-2.20)。在非匹配队列中,18-49 岁患者使用 HM3 的存活率与 OHT 相当(96.9% vs 95.9%,N = 91,P = 1.00;RR = 0.92,95% CI = [0.09-9.78]);50 岁以上患者使用 HM3 的存活率相似,尽管有 8.9% 的差异(75.0% vs 83.9%,N = 290,P = 0.60;RR = 1.51,95% CI = [0.85-2.68])。结论这项探索性分析表明,作为心衰的主要治疗方法,对于类似患者,HM3的3年生存率可能与OHT相当,但可能导致更多的再入院率。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


