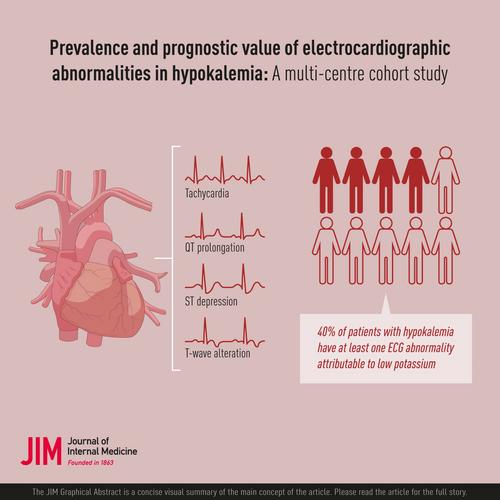
Prevalence and prognostic value of electrocardiographic abnormalities in hypokalemia: A multicenter cohort study
Abstract
Background
Hypokalemia is common in hospitalized patients and associated with ECG abnormalities. The prevalence and prognostic value of ECG abnormalities in hypokalemic patients are, however, not well established.
Methods
The study was a multicentered cohort study, including all ault patients with an ECG and potassium level <4.4 mmol/L recorded at arrival to four emergency departments in Denmark and Sweden. Using computerized measurements from ECGs, we investigated the relationship between potassium levels and heart rate, QRS duration, corrected QT (QTc) interval, ST-segment depressions, T-wave flattening, and T-wave inversion using cubic splines. Within strata of potassium levels, we further estimated the hazard ratio (HR) for 7-day mortality, admission to the intensive care unit (ICU), and diagnosis of ventricular arrhythmia or cardiac arrest, comparing patients with and without specific ECG abnormalities matched 1:2 on propensity scores.
Results
Among 79,599 included patients, decreasing potassium levels were associated with a concentration-dependent increase in all investigated ECG variables. ECG abnormalities were present in 40% of hypokalemic patients ([K+] <3.5 mmol/L), with T-wave flattening, ST-segment depression, and QTc prolongation occurring in 27%, 16%, and 14%. In patients with mild hypokalemia ([K+] 3.0–3.4 mmol/L), a heart rate >100 bpm, ST-depressions, and T-wave inversion were associated with increased HRs for 7-day mortality and ICU admission, whereas only a heart rate >100 bpm predicted both mortality and ICU admission among patients with [K+] <3.0 mmol/L. HR estimates were, however, similar to those in eukalemic patients. The low number of events with ventricular arrhythmia limited evaluation for this outcome.
Conclusions
ECG abnormalities were common in hypokalemic patients, but they are poor prognostic markers for short-term adverse events under the current standard of care.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


