Challenges hindering emergency physicians; involvement in multicenter collaborative studies in Japan: A nationwide survey analysis
Abstract
Aim
Multicenter collaborative research accelerates patient recruitment and strengthens evidence. Nevertheless, the factors influencing emergency and critical care physicians’ involvement in such research in Japan remain unclear.
Methods
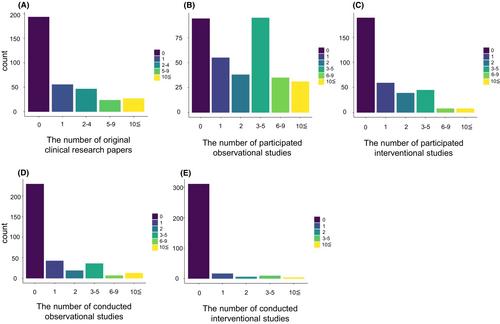
A nationwide web-based survey conducted in early 2023 targeted emergency physicians working a minimum of 3 days per week in Japan. The survey descriptively assessed their backgrounds, work and research environments, experiences, and perceived impediments and motivators for multicenter research.
Results
Of the 387 respondents, 348 were included in the study, yielding a 5.1% response rate. Women comprised 11% of the participants; 33% worked in university hospitals, 65% served in both emergency departments and intensive care units, and 54% did shift work. Only 12% had designated research time during working hours, with a median of 1 hour per week (interquartile range 0–5 h), including time outside of work. While 73% had participated in multicenter research, 58% noted barriers to participation. The key obstacles were excessive data entry (72%), meeting time constraints (59%), ethical review at each facility (50%), and unique sample collection, such as bronchoalveolar lavage specimens or pathological tissues (51%). The major incentives were networking (70%), data sets reuse (65%), feedback on research results (63%), and recognition from academic societies (63%). Financial rewards were not highly prioritized (38%).
Conclusions
While valuing clinical research, emergency physicians face barriers, especially data entry burden and limited research time. Networking and sharing research findings motivate them. These insights can guide strategies to enhance collaborative research in emergency and critical care in Japan.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


