Viral N Shah, Shijing Qui, Jason Stoneback, Lubna Qamar, Virginia L Ferguson, Wendy M Kohrt, Janet K Snell-Bergeon, Sudhaker D Rao
{"title":"Bone Structure and Turnover in Postmenopausal Women With Long-Standing Type 1 Diabetes","authors":"Viral N Shah, Shijing Qui, Jason Stoneback, Lubna Qamar, Virginia L Ferguson, Wendy M Kohrt, Janet K Snell-Bergeon, Sudhaker D Rao","doi":"10.1002/jbm4.10831","DOIUrl":null,"url":null,"abstract":"<p>Compromised bone structural and mechanical properties are implicated in the increased fracture risk in type 1 diabetes (T1D). We investigated bone structure and turnover by histomorphometry in postmenopausal women with T1D and controls without diabetes using tetracycline double-labeled transiliac bone biopsy. After in vivo tetracycline double labeling, postmenopausal women with T1D of at least 10 years and without diabetes underwent transiliac bone biopsy. An expert blinded to the study group performed histomorphometry. Static and dynamic histomorphometry measurements were performed and compared between the two groups. The analysis included 9 postmenopausal women with T1D (mean age 58.4 ± 7.1 years with 37.9 ± 10.9 years of diabetes and HbA1c 7.1% ± 0.4%) and 7 postmenopausal women without diabetes (mean age 60.9 ± 3.3 years and HbA1c 5.4% ± 0.2%). There were no significant differences in serum PTH (38.6 ± 8.1 versus 51.9 ± 23.9 pg/mL), CTX (0.4 ± 0.2 versus 0.51 ± 0.34 ng/mL), or P1NP (64.5 ± 26.2 versus 87.3 ± 45.3 ng/mL). Serum 25-hydroxyvitamin D levels were higher in T1D than in controls (53.1 ± 20.8 versus 30.9 ± 8.2 ng/mL, <i>p</i> < 0.05). Bone structure metrics (bone volume, trabecular thickness, trabecular number, and cortical thickness) were similar between the groups. Indices of bone formation (osteoid volume, osteoid surface, and bone formation rate) were 40% lower in T1D and associated with lower activation frequency. However, the differences in bone formation were not statistically significant. Long-standing T1D may affect bone turnover, mainly bone formation, without significantly affecting bone structure. Further research is needed to understand bone turnover and factors affecting bone turnover in people with T1D. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC. on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 11","pages":""},"PeriodicalIF":3.4000,"publicationDate":"2023-10-15","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10831","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10831","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0
Abstract
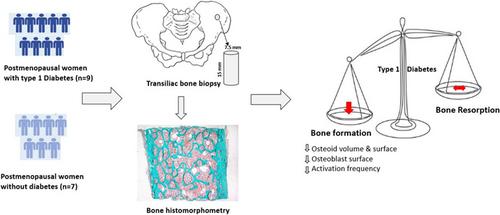
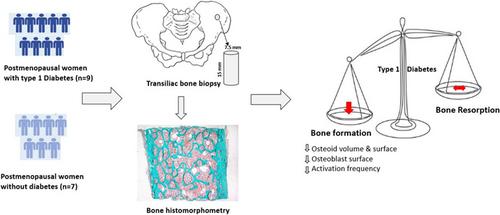
Compromised bone structural and mechanical properties are implicated in the increased fracture risk in type 1 diabetes (T1D). We investigated bone structure and turnover by histomorphometry in postmenopausal women with T1D and controls without diabetes using tetracycline double-labeled transiliac bone biopsy. After in vivo tetracycline double labeling, postmenopausal women with T1D of at least 10 years and without diabetes underwent transiliac bone biopsy. An expert blinded to the study group performed histomorphometry. Static and dynamic histomorphometry measurements were performed and compared between the two groups. The analysis included 9 postmenopausal women with T1D (mean age 58.4 ± 7.1 years with 37.9 ± 10.9 years of diabetes and HbA1c 7.1% ± 0.4%) and 7 postmenopausal women without diabetes (mean age 60.9 ± 3.3 years and HbA1c 5.4% ± 0.2%). There were no significant differences in serum PTH (38.6 ± 8.1 versus 51.9 ± 23.9 pg/mL), CTX (0.4 ± 0.2 versus 0.51 ± 0.34 ng/mL), or P1NP (64.5 ± 26.2 versus 87.3 ± 45.3 ng/mL). Serum 25-hydroxyvitamin D levels were higher in T1D than in controls (53.1 ± 20.8 versus 30.9 ± 8.2 ng/mL, p < 0.05). Bone structure metrics (bone volume, trabecular thickness, trabecular number, and cortical thickness) were similar between the groups. Indices of bone formation (osteoid volume, osteoid surface, and bone formation rate) were 40% lower in T1D and associated with lower activation frequency. However, the differences in bone formation were not statistically significant. Long-standing T1D may affect bone turnover, mainly bone formation, without significantly affecting bone structure. Further research is needed to understand bone turnover and factors affecting bone turnover in people with T1D. © 2023 The Authors. JBMR Plus published by Wiley Periodicals LLC. on behalf of American Society for Bone and Mineral Research.
长期患有1型糖尿病的绝经后妇女的骨结构和代谢
1型糖尿病(T1D)患者骨折风险增加与骨骼结构和力学特性受损有关。我们使用四环素双标记经髂骨活检,通过组织形态学测量研究了绝经后T1D妇女和无糖尿病的对照组的骨结构和转换。在体内四环素双标记后,绝经后T1D至少10年且无糖尿病的妇女进行了经髂骨活检。一位对研究组不知情的专家进行了组织形态学测定。在两组之间进行静态和动态组织形态测量并进行比较。分析包括9名绝经后T1D妇女(平均年龄58.4±7.1岁,糖尿病37.9±10.9年,HbA1c 7.1%±0.4%)和7名绝经后无糖尿病妇女(平均年龄60.9±3.3岁,HbA1c 5.4%±0.2%)。血清PTH(38.6±8.1 vs . 51.9±23.9 pg/mL)、CTX(0.4±0.2 vs . 0.51±0.34 ng/mL)、P1NP(64.5±26.2 vs . 87.3±45.3 ng/mL)差异无统计学意义。T1D患者血清25-羟基维生素D水平高于对照组(53.1±20.8 ng/mL vs 30.9±8.2 ng/mL, p < 0.05)。骨结构指标(骨体积、骨小梁厚度、骨小梁数量和皮质厚度)在两组之间相似。T1D患者的骨形成指标(类骨体积、类骨表面和骨形成率)降低40%,且与较低的激活频率相关。然而,骨形成的差异没有统计学意义。长期存在的T1D可能影响骨转换,主要是骨形成,但对骨结构没有明显影响。需要进一步研究了解T1D患者的骨转换及影响骨转换的因素。©2023作者。JBMR Plus由Wiley期刊有限责任公司代表美国骨与矿物研究协会出版。
本文章由计算机程序翻译,如有差异,请以英文原文为准。

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


