Endovascular Stent Graft Treatment of an Iatrogenic Symptomatic Extracranial Carotid-Jugular Arteriovenous Fistula.
IF 0.8
Q4 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
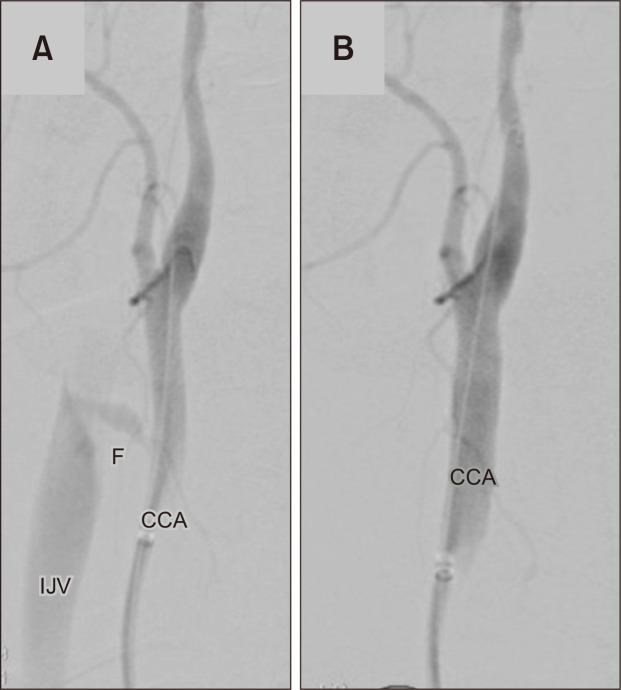
Trauma is a major health concern, and despite the development of solid trauma systems, the associated morbidity and mortality continue to rise [1]. Cervical trauma, in particular, is notoriously difficult to treat, mainly because of the complex anatomy in a narrow anatomic space. Due to its multiple mechanisms and locations, surgical techniques can also be highly variable. In Zone II cervical vascular injuries, open surgical repair is the norm due to its feasibility, ability to explore other cervical structures and relatively low risks when compared to other proximal or distal locations [2,3]. However, in highly-unstable patients, a lengthy procedure with risks of severe hemorrhage can offset a successful outcome, when compared to an endovascular approach. We describe the case of a 56-year-old male admitted in critical care for septic shock due to severe pneumonia, along with acute renal failure. After an inadvertent right carotid puncture during an attempt to place a temporary dialysis catheter in the internal jugular vein, he developed sudden hemodynamic and ventilatory deterioration. He also presented a carotid bruit and neck engorgement. Ultrasound revealed a right common carotid–internal jugular arteriovenous fistula and allowed precise location marking, as well as the measurement of the diameter and proximal and distal seal lengths (proximal to the carotid bifurcation). Due to the unfavorable neck anatomy and high surgical risk, endovascular treatment was preferred. Right femoral access was used, and unfractionated heparin administered. After selective catheterization of the innominate artery and angiographic marking the fistula and carotid side branches (Fig. 1A), a covered stentgraft 9 mm×38 mm (Advanta V12; Atrium Medical Corp., Hudson, NH, USA) was successfully deployed, covering the fistula without branch compromise (Fig. 1B). The procedure required 25 minutes and 20 mL of iodinated contrast. The patient experienced immediate relief of the hemodynamic and ventilatory burden of the fistula; however, he was unable to withstand the severity of his underlying pathology and died after a prolonged hospitalization (41 days). Im ge of Vacular Srgery Endovascular Stent Graft Treatment of an Iatrogenic Symptomatic Extracranial Carotid-Jugular Arteriovenous Fistula
血管内支架移植治疗医源性症状性颅外颈颈动静脉瘘。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Vascular Specialist International
Medicine-Surgery
CiteScore
1.10
自引率
11.10%
发文量
29
审稿时长
17 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


