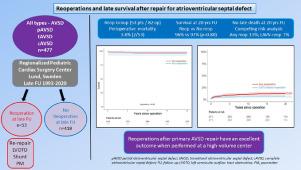
Reoperations After Repair for Atrioventricular Septal Defects: >25 Years Experience at a Single Center
Abstract
Our aim was to evaluate the total burden of reoperations after previous repair for atrioventricular septal defects, including long-term survival and identify risk factors for reoperation. All patients with surgical correction for atrioventricular septal defect (AVSD) 1993- 2020 underwent a follow-up in October 2020. Clinical data were obtained by retrospective review and evaluated with Kaplan-Meier and competing risk analysis. Of 477 patients who underwent initial repair, 53 patients (11.1%) underwent a total of 82 reoperations. The perioperative mortality at reoperation was 3.8% (2/53). There were no late deaths (0/51) during follow-up. In patients requiring reoperation for left atrioventricular valve regurgitation, a re-repair was performed in 90% (26/29) at first attempt. Estimated overall survival was 96.2 ± 2.6% (95% CI 91.2-100) in the Any reoperation group and 96.7 ± 0.9% (95% CI 94.9-98.5) in the No reoperation group at 20 years (P = 0.80). The cumulative incidence function of Any reoperation (with death as competing risk) was 13.0% (95% CI 9.4-16.5) at 20 years. Independent risk factors for Any reoperation included severe mitral regurgitation after primary repair (HR 40.7; 95% CI 14.9-111; P < 0.001). The risk of perioperative mortality in AVSD patients undergoing reoperation was low in the present study. Long-term survival was very good and not significantly different when compared to patients who did not need reoperation. Re-repair for left atrioventricular valve regurgitation was possible in most cases and showed long-term durability. Our data suggest that reoperations after primary repair of AVSD have very good long-term outcomes when performed at a high-volume pediatric cardiac surgery center.

| 公司名称 | 产品信息 | 采购帮参考价格 |
|---|
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


