Association between acculturation, dental floss use, dental visits and unmet dental needs among Asians in the United States: Findings from National Health and Nutrition Examination Survey (NHANES) 2011–2018
Abstract
Objectives
The objectives of this study were to examine the associations between acculturation and dental floss, regular dental visits and unmet dental care needs among Asian Americans, as well as the moderating effects of these associations.
Methods
This study analysed national representative samples from the National Health and Nutrition Examination Survey (NHANES) 2011–2018. A total of 2763 Asian Americans aged 20 and older were included in this analysis. The primary predictor, acculturation score, was determined by three questions: (i) language spoken at home (higher score for English), (ii) country of birth (higher score for United States) and (iii) length of time in the United States. Dental floss use, dental visits and unmet dental care needs were included as outcomes in this study. Descriptive statistics and logistic regressions were used to analyse the samples.
Results
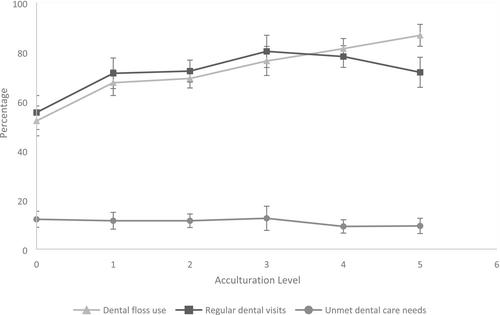
Acculturation was significantly associated with dental health behaviours: Individuals with higher levels of acculturation were more likely than less acculturated individuals to use dental floss (81.0% vs. 63.9%, respectively) and visit the dentist regularly (76.7% vs. 66.9% respectively). Insurance status moderated the association between acculturation and dental visits: Acculturation was significantly associated with dental visits in the past year among insured individuals (OR = 1.70, 95% CI: 1.29–2.23), but not among uninsured individuals. Unmet dental care needs were present in 11.1% of participants. While costs and insurance were the top two determinants of access to care, individuals with and without insurance differed with regard to their third major reason for unmet dental care needs: Being ‘too busy’ and not wanting to spend money on dental care.
Conclusions
Among the Asian population in the United States, those with high acculturation scores were more likely to engage in dental flossing and visit the dentist regularly compared to those Asians with lower acculturation scores. To encourage dental flossing and regular dental visits among Asians with lower acculturation scores, cultural adaptation and language accessibility suggests being considered. Future research is necessary to confirm the moderating effect of insurance status on the association between acculturation and regular dental visits. Additionally, our findings emphasize the impact of costs and insurance on access to dental care among Asians in the United States, highlighting the importance of future public health programmes in addressing these barriers.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


