Valve positions upon which cardiac surgeons operate should be taken into consideration.
IF 2.2
4区 医学
Q2 SURGERY
引用次数: 0
Abstract
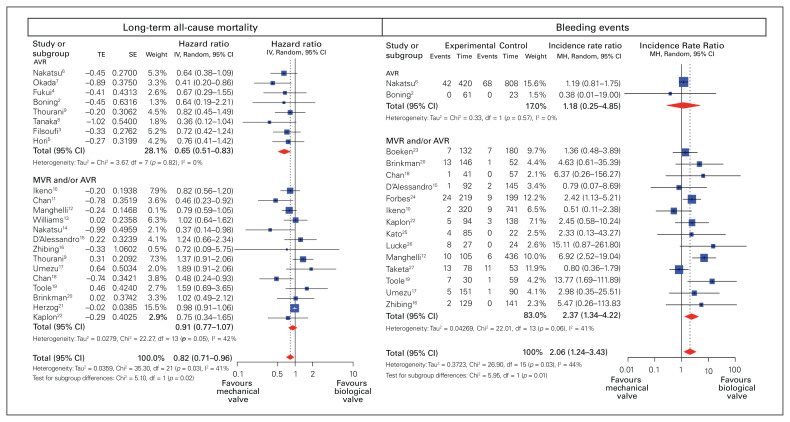
We read the art ic le entit led “Mechanical versus bioprosthetic valves in chronic dialysis: a systematic review and meta-analysis” by Kim and colleagues,1 with great interest. The authors attempted to address limitations of previous meta-analyses by expanding the searching strategy and exhausting more databases without placing any language restriction. They concluded that the significant benefit of lower all-cause mortality with the use of mechanical prosthesis (MP) was at the expense of higher risks of bleeding and stroke. We appreciated the authors’ efforts and contribution, and concur with the authors that most studies were subject to high risk of unmeasured confounding bias owing to unreported demographics, which lowers the quality of evidence considerably. However, we believe that the prosthetic position upon which cardiac surgeons operate is a significant contributor to not only conceptual, but also statistical heterogeneity. Besides, compared with relative risk (RR) that Kim and colleagues selected for the analysis of all-cause mortality, hazard ratio (HR) is supposed to be a more appropriate statistic, as it incorporates time into the consideration. Thus, we followed Kim and colleagues’ inclusion criteria and reconducted the meta-analysis with the introduction of a subgroup analysis based on valve position. There are 8 studies2–9 providing comparative long-term survival outcome for aortic valve replacement (AVR) between MP and bioprosthesis (BP) in dialysis patients. We showed that dialysis patients using MP for AVR was associated with significantly lower longterm all-cause mortality than those using BP (HR 0.65, 95 % confidence interval [CI] 0.51–0.83, I2 = 0 %) (Figure 1). On the other hand, the long-term overall survival was comparable between MP and BP (HR 0.91, 95 % CI 0.77–1.07, I2 = 0 %) (Figure 1) in mixed cohorts of AVR and mitral valve replacement (MVR). Regarding the bleeding events, although the use of MP was associated with a considerably higher risk in studies including mixed cohorts of AVR and MVR (incidence rate ratio [IRR] 2.37, 95% CI 1.34–4.22, I2 = 41%), we found that there was no significant difference in bleeding events between MP and BP in patients undergoing AVR (IRR 1.18, 95% CI 0.28–4.85, I2 = 0 %) (Figure 1). One plausible explanation for similar bleeding risk between MP and BP in dialysis patients undergoing AVR may reside in the lower target of international normalized ratio (INR), usual ly less than 2.5, used in this popu lation, as compared with the target of 3.0 used in MVR.28 In fact, it LETTERS • LETTRES
心脏外科医生手术时应考虑到瓣膜的位置。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
3.00
自引率
8.00%
发文量
120
审稿时长
6-12 weeks
期刊介绍:
The mission of CJS is to contribute to the meaningful continuing medical education of Canadian surgical specialists, and to provide surgeons with an effective vehicle for the dissemination of observations in the areas of clinical and basic science research.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


