Bilateral Isolated Common and Internal Iliac Artery Aneurysms Treated with Iliac Branch Endoprostheses Using the Gluteal Arteries as Distal Landing Zones.
IF 0.8
Q4 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
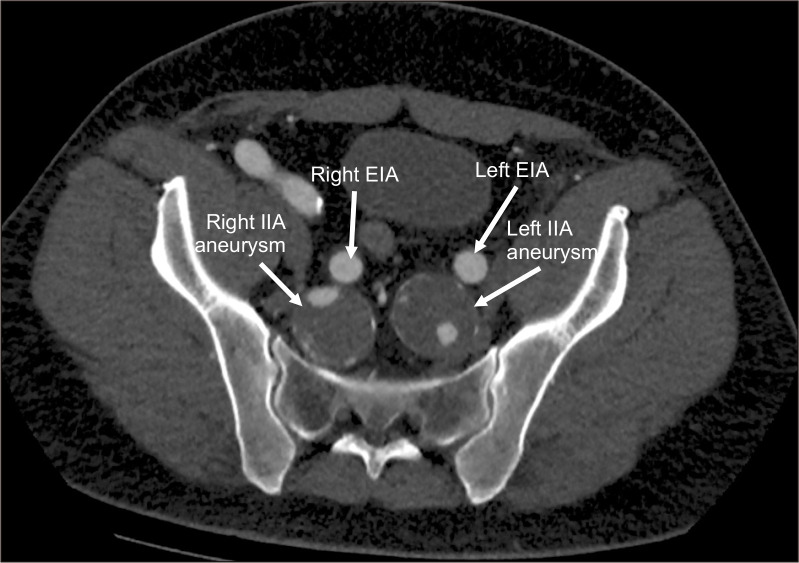
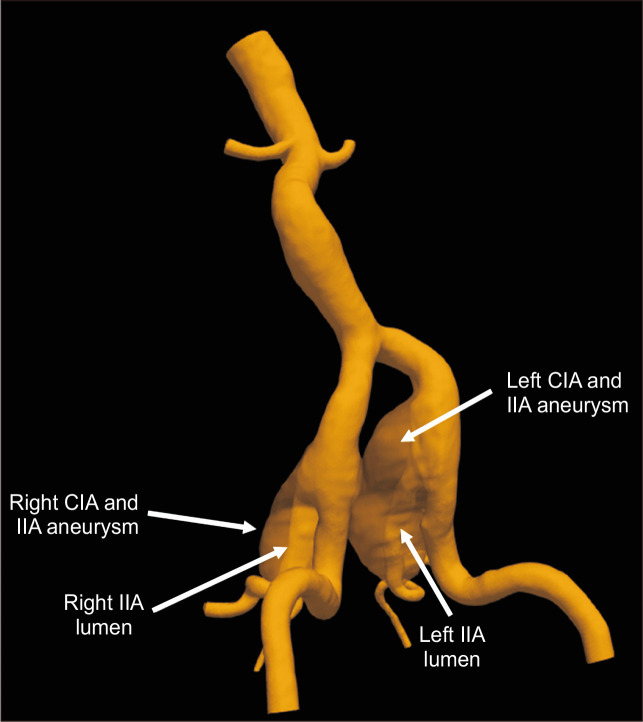
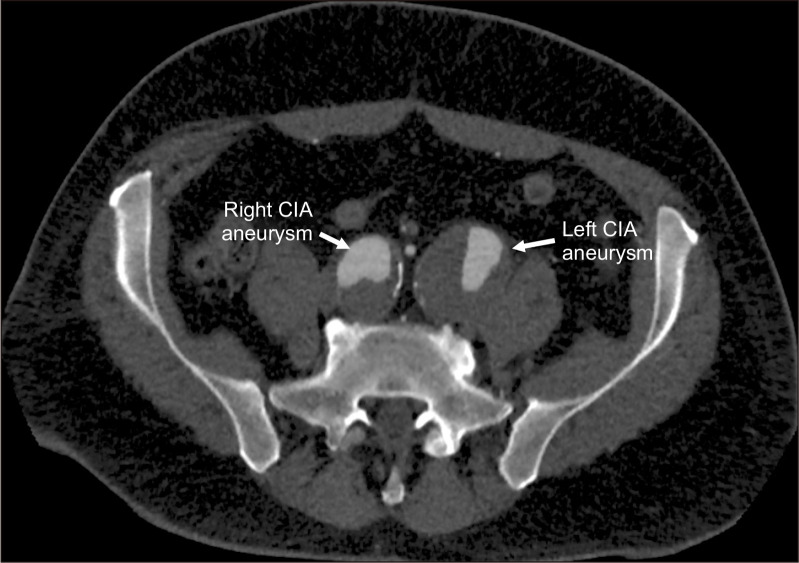
A 52-year-old male presented with bilateral isolated type III, 45-mm common and internal iliac artery (CIA and IIA) aneurysms (Fig. 1, 2) [1]. Both the CIAs exhibited an adequate proximal non-aneurysmatic segment, whereas the IIAs were aneurysmatic throughout their length (Fig. 3, 4). The patient underwent percutaneous endovascular treatment using iliac branch endoprosthesis (IBE) systems bilaterally (W. L. Gore and Associates, Inc.). The right superior and left inferior gluteal arteries were used as distal landing zones, as these presented lesser tortuosity than did the right inferior and left superior gluteal arteries, which were embolized before IBE deployment with 7-mm coils. Initially, self-expandable covered stents (Viabahn 9×100 mm; W. L. Gore & Associates, Inc.) were placed distally within the target vessels to better conform their anatomy. Subsequently, these stents were connected to the internal iliac leg of the IBE with balloon-expandable covered stents (VBX 11×79 mm; W. L. Gore & Associates, Inc.). The patient’s postoperative course was uneventful, with immediate mobilization Im ge of Vacular Srgery Bilateral Isolated Common and Internal Iliac Artery Aneurysms Treated with Iliac Branch Endoprostheses Using the Gluteal Arteries as Distal Landing Zones
以臀动脉为远端着陆区髂支假体治疗双侧孤立髂总动脉和髂内动脉瘤。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Vascular Specialist International
Medicine-Surgery
CiteScore
1.10
自引率
11.10%
发文量
29
审稿时长
17 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


