Neuropathies Following an Ultrasound-Guided Axillary Brachial Plexus Block.
IF 1.9
Q3 ANESTHESIOLOGY
引用次数: 0
Abstract
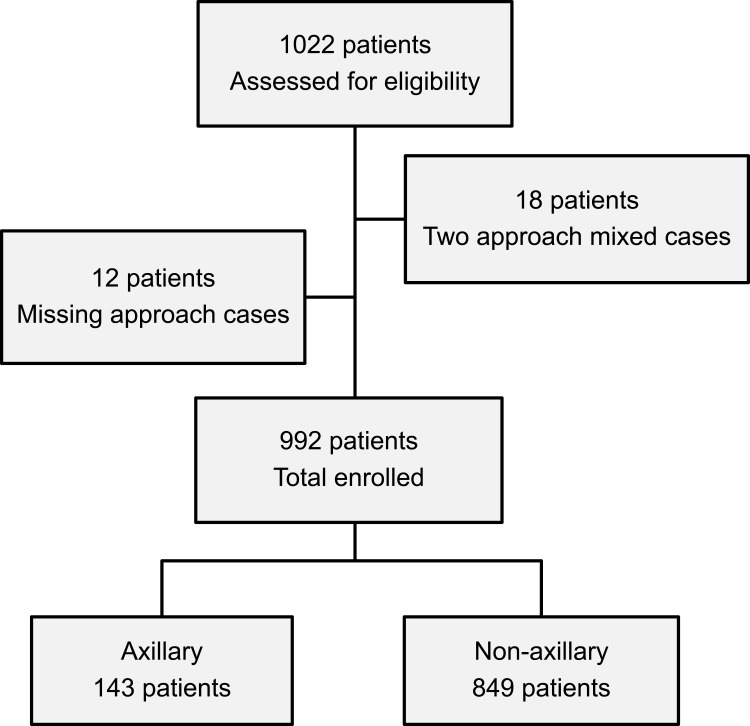
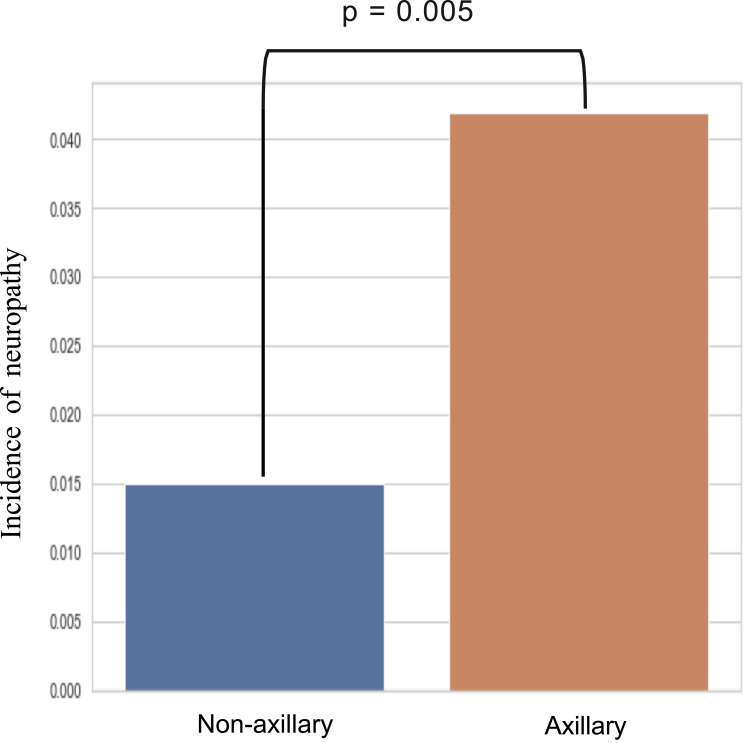
Purpose Ultrasound-guided brachial plexus block (UGBPB) has interscalene, supraclavicular, infraclavicular, and axillary approaches. The axillary block is considered to be the safest and with fewer adverse events compared to the interscalene (eg, phrenic nerve block, spinal cord or vertebral artery puncture) and supraclavicular (eg, pneumothorax). However, with regard to postoperative neurological symptoms (PONS), it is controversial whether its incidence after an axillary block was higher than that after non-axillary approaches”. In this study, we investigated whether the incidence of a neuropathy after an axillary block was higher than that after non-axillary approaches. Patients and Methods This was a single-center, retrospective cohort study. All UGBPBs were performed under general anesthesia between January 2014 and March 2020. The outcomes included the overall incidence of PONS and neuropathies for axillary and non-axillary approaches. The etiology, symptoms, and outcomes of patients were investigated. Results Of the 992 patients, 143 (14%) and 849 (86%) were subjected to axillary and non-axillary approaches, respectively. Among 19 cases (19.2:1000; 95% confidence interval [CI], 18.2–20.1) of PONS, four (4.0:1000; 95% CI, 3.8–4.2) were neuropathies attributed to the UGBPB, three (21.0:1000; 95% CI, 18.1–23.8) to the axillary and one (2.8:1000; 95% CI, 2.6–3.1) to non-axillary approaches. The incidence of neuropathies after an axillary block was significantly higher than that after non-axillary approaches (P = 0.005). Conclusion The incidence of neuropathies after US-guided axillary block under general anesthesia was significantly higher than that after non-axillary approaches.
超声引导下腋窝臂丛神经阻滞后的神经病变。
目的:超声引导下臂丛阻滞(UGBPB)有斜角肌间、锁骨上、锁骨下和腋窝入路。与斜角肌间(如膈神经阻滞、脊髓或椎动脉穿刺)和锁骨上(如气胸)相比,腋窝阻滞被认为是最安全的,不良事件较少。然而,关于术后神经系统症状(PONS),腋路阻滞后的发生率是否高于非腋路入路仍存在争议”。在这项研究中,我们调查了腋窝阻滞后神经病变的发生率是否高于非腋窝入路。患者和方法:这是一项单中心、回顾性队列研究。所有UGBPBs均于2014年1月至2020年3月在全身麻醉下进行。结果包括腋窝和非腋窝入路的PONS和神经病变的总发生率。对患者的病因、症状和预后进行了调查。结果:992例患者中,143例(14%)采用腋窝入路,849例(86%)采用非腋窝入路。19例中(19.2:1000;PONS的95%置信区间[CI], 18.2-20.1), 4例(4.0:1000;95% CI, 3.8-4.2)为UGBPB所致神经病,3例(21.0:1000;95% CI, 18.1-23.8)和1 (2.8:1000;95% CI, 2.6-3.1)到非腋窝入路。腋窝入路后神经病变发生率明显高于非腋窝入路(P = 0.005)。结论:全麻下us引导下腋窝阻滞术后神经病变的发生率明显高于非腋窝入路。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


