Predictors of Clinical Nurse Leader implementation success across a national sample of settings: A Bayesian multilevel modeling analysis
Abstract
Introduction
The Clinical Nurse Leader (CNL) care model is a different way of organizing frontline nursing care delivery in contrast to the traditional “staff nurse” model and is increasingly being adopted by health systems across the United States and abroad. However, variability in implementation and outcomes has been noted across health settings.
Aim
A recently validated CNL Practice Model provides an explanatory pathway for CNL model integration into practice. The purpose of this study was to identify and compare patterns of empirical correspondence to the CNL Practice Model and predict their influence on implementation success.
Methods
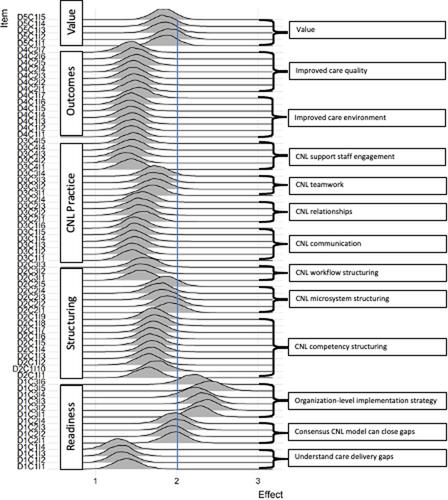
We conducted a secondary analysis of a 2015 national-level study with clinicians and administrators involved with CNL initiatives in their health system. A psychometrically validated CNL Practice Survey was used to collect data measuring the presence (0%–100%) of the five domains of the CNL Practice Model (organizational readiness, CNL structuring, CNL practices, outcomes, and value) and one measure of CNL implementation success. We modeled the complex hierarchical structure of the data using a Bayesian multilevel regression mixed modeling approach. A zero–one-inflated beta distribution, a mixture of Bernoulli distributions for the minimum and maximum responses and a beta distribution for the responses between the minimum and maximum, was used to fit success ratings in the model.
Results
A total of 920 participants responded, 540 (59%) provided success scores. The model captured ratings skewed toward upper bound, while also adequately modeling data between the minimum and maximum values. The Bayesian model converged and gave estimates for all hierarchical parameters, which would likely have failed to converge in a pure maximum likelihood framework. The variability around success score across CNL Practice Model element ratings was greatest at the component level, 0.29 (0.18–0.48), compared to either the domain level, 0.16 (0.01–0.54), or the item level, 0.09 (0.01–0.17). The components most predictive of implementation success were (a) consensus CNL model can close gaps, (b) organization level implementation strategy, and (c) alignment of empirical CNL microsystem level structuring to the model's conceptualization.
Conclusions
Findings provide further empirical evidence to support the explanatory pathway proposed by the CNL Practice Model and identified specific organizational readiness and CNL workflow structures that are critical antecedents predictive of CNL practice manifestation and production of expected outcomes. Findings indicate actionable implementation evidence that can be successfully adopted across real-world healthcare settings to achieve safer and higher quality patient care.
Clinical Relevance
CNL integrated care delivery is a frontline nursing care model that is being increasingly adopted by health systems across the United States and abroad. However, variability in CNL implementation and outcomes has been noted across health settings, limiting its evidence base. Findings of this study contribute a better understanding about the variability of CNL practice and outcomes found in the literature and contribute empirical and conceptual clarity about the relationships between modes of CNL implementation and successful adoption in healthcare settings.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


