糖尿病患者肾病的综合疗法
IF 28.6
1区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
摘要
糖尿病肾病(DKD)是指在没有其他明确肾损伤原因的情况下,同时存在糖尿病和慢性肾病,约 20-40% 的糖尿病患者会出现这种疾病。随着全球糖尿病患病率的上升,慢性肾脏病也变得非常普遍,成为导致肾衰竭、心血管疾病加速、过早死亡和全球医疗支出的主要原因。多种病理生理机制导致了 DKD,而单一的生活方式或药物干预对保护肾功能的效果有限。近二十年来,肾素-血管紧张素系统抑制剂是唯一可用的肾脏保护药物。然而,包括钠葡萄糖共转运体-2 抑制剂、一种非甾体类矿物皮质激素拮抗剂和一种选择性内皮素受体拮抗剂在内的几类新药现已被证明可改善 2 型糖尿病患者的肾脏预后。此外,新出现的胰高血糖素样肽-1 受体激动剂肾脏保护作用的临床前和临床证据也促使人们对这些药物进行前瞻性试验,以治疗 DKD。研究和临床工作的目标是将具有潜在互补疗效的疗法联合使用,以安全地阻止肾脏疾病的进展。随着更多肾脏保护药物的问世,DKD 患者的前景在未来几十年应该会有所改善。本文章由计算机程序翻译,如有差异,请以英文原文为准。
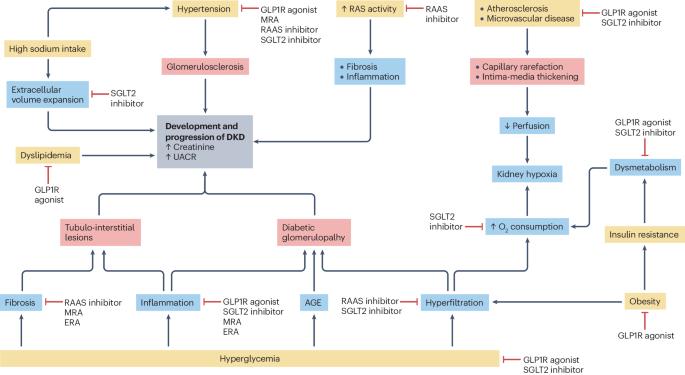
Combination therapy for kidney disease in people with diabetes mellitus
Diabetic kidney disease (DKD), defined as co-existing diabetes and chronic kidney disease in the absence of other clear causes of kidney injury, occurs in approximately 20–40% of patients with diabetes mellitus. As the global prevalence of diabetes has increased, DKD has become highly prevalent and a leading cause of kidney failure, accelerated cardiovascular disease, premature mortality and global health care expenditure. Multiple pathophysiological mechanisms contribute to DKD, and single lifestyle or pharmacological interventions have shown limited efficacy at preserving kidney function. For nearly two decades, renin–angiotensin system inhibitors were the only available kidney-protective drugs. However, several new drug classes, including sodium glucose cotransporter-2 inhibitors, a non-steroidal mineralocorticoid antagonist and a selective endothelin receptor antagonist, have now been demonstrated to improve kidney outcomes in people with type 2 diabetes mellitus. In addition, emerging preclinical and clinical evidence of the kidney-protective effects of glucagon-like-peptide-1 receptor agonists has led to the prospective testing of these agents for DKD. Research and clinical efforts are geared towards using therapies with potentially complementary efficacy in combination to safely halt kidney disease progression. As more kidney-protective drugs become available, the outlook for people living with DKD should improve in the next few decades. Several new drug classes have been demonstrated to improve kidney outcomes in people with diabetes mellitus. Here, the authors examine the evidence for the efficacy and safety of combination treatment to reduce the progression of diabetic kidney disease.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Nature Reviews Nephrology
医学-泌尿学与肾脏学
CiteScore
39.00
自引率
1.20%
发文量
127
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Nephrology aims to be the premier source of reviews and commentaries for the scientific communities it serves.
It strives to publish authoritative, accessible articles.
Articles are enhanced with clearly understandable figures, tables, and other display items.
Nature Reviews Nephrology publishes Research Highlights, News & Views, Comments, Reviews, Perspectives, and Consensus Statements.
The content is relevant to nephrologists and basic science researchers.
The broad scope of the journal ensures that the work reaches the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


