Extraspinal sacrococcygeal myxopapillary ependymoma in a teenager.
IF 1
Q3 MEDICINE, GENERAL & INTERNAL
Journal of Yeungnam medical science
Pub Date : 2023-10-01
Epub Date: 2022-09-02
DOI:10.12701/jyms.2022.00367
引用次数: 0
Abstract
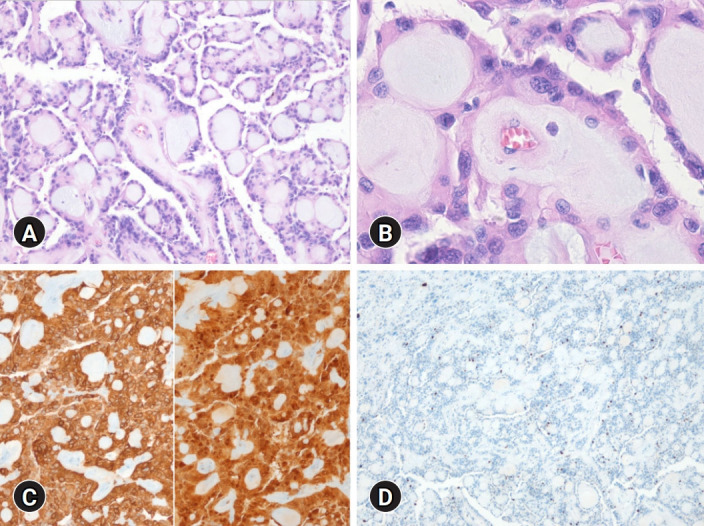
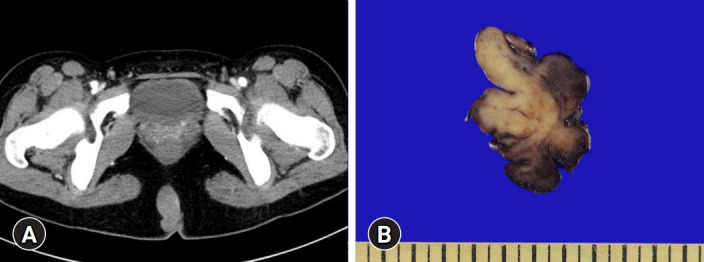
school, the patient was prescribed antibiotics and surgery was planned during her vacation. Two months later, she underwent computed tomography which revealed a well-demarcated solid mass in the intragluteal fold area, which did not show any connection to the sacrum (Fig. 1A). These findings suggested tumors such as extraspinal sacrococcygeal myxopapillary ependymoma (ESME) rather than inflammatory changes. Elective surgery was performed, which revealed a multilobulated fleshy mass, measuring approximately 5.9 × 3.6 cm ( Fig. 1B). On histologic examination, the tumor was well-demarcated by a fibrous capsule and composed of papillary structures with fibrovascular cores and myxoid materials, with relatively monomorphic tumor cells arranged along the papillary wall. In some areas, focal pleomorphic cells were identified but the highest mitotic count was 1/mm. No necrosis or microvascular proliferation was observed. Immunohistochemical staining for GFAP and S100 protein was positive for tumor cells, but cytokeratin was negative and the Ki-67 index was less than 1% (Fig. 2). These features were consistent with ESME. On follow-up, brain and spine magnetic resonance imaging showed no metastasis or recurrence. ESME is a rare glial tumor, and presented in an unusual location in our case. Since the first case reported by Mallory [1], less than 50 cases occurring in childhood have been reported in the literature [2]. Because of its rarity, the tumor is sometimes misdiagnosed as pilonidal abscess or detected only after treatment, includ-
青少年骶尾部脊髓外黏液乳头状室管膜瘤。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


