OrthoMortPred: Predicting one-year mortality following orthopedic hospitalization
IF 3.7
2区 医学
Q2 COMPUTER SCIENCE, INFORMATION SYSTEMS
International Journal of Medical Informatics
Pub Date : 2024-10-18
DOI:10.1016/j.ijmedinf.2024.105657
引用次数: 0
Abstract
Objective
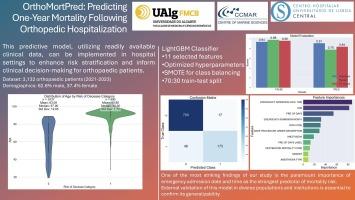
Predicting mortality risk following orthopedic surgery is crucial for informed decision-making and patient care. This study aims to develop and validate a machine learning model for predicting one-year mortality risk after orthopedic hospitalization and to create a personalized risk prediction tool for clinical use.
Methods
We analyzed data from 3,132 patients who underwent orthopedic procedures at the Central Lisbon University Hospital Center from 2021 to 2023. Using the LightGBM algorithm, we developed a predictive model incorporating various clinical and administrative variables. We employed SHAP (SHapley Additive exPlanations) values for model interpretation and created a personalized risk prediction tool for individual patient assessment.
Results
Our model achieved an accuracy of 93% and an area under the ROC curve of 0.93 for predicting one-year mortality. Notably, ’EMERGENCY ADMISSION DATE TIME’ emerged as the most influential predictor, followed by age and pre-operative days. The model demonstrated robust performance across different patient subgroups and outperformed traditional statistical methods. The personalized risk prediction tool provides clinicians with real-time, patient-specific risk assessments and insights into contributing factors.
Conclusion
Our study presents a highly accurate model for predicting one-year mortality following orthopedic hospitalization. The significance of ’EMERGENCY ADMISSION DATE TIME’ as the primary predictor highlights the importance of admission timing in patient outcomes. The accompanying personalized risk prediction tool offers a practical means of implementing this model in clinical settings, potentially improving risk stratification and patient care in orthopedic practice.
OrthoMortPred:预测骨科住院后一年的死亡率。
目的:预测骨科手术后的死亡风险对于知情决策和患者护理至关重要。本研究旨在开发和验证一个机器学习模型,用于预测骨科住院后一年的死亡风险,并创建一个供临床使用的个性化风险预测工具:我们分析了2021年至2023年期间在里斯本中央大学医院中心接受骨科手术的3132名患者的数据。我们使用 LightGBM 算法开发了一个包含各种临床和管理变量的预测模型。我们采用 SHAP(SHapley Additive exPlanations)值来解释模型,并创建了一个个性化的风险预测工具,用于对患者进行个体评估:我们的模型预测一年死亡率的准确率为 93%,ROC 曲线下面积为 0.93。值得注意的是,"急诊入院日期时间 "是最有影响力的预测因素,其次是年龄和术前天数。该模型在不同的患者亚群中表现稳健,优于传统的统计方法。个性化风险预测工具为临床医生提供了实时的、针对特定患者的风险评估,以及对诱因的深入了解:我们的研究提出了一个高度准确的模型,用于预测骨科住院一年后的死亡率。急诊入院日期时间 "作为主要预测因素的重要性凸显了入院时间对患者预后的重要性。随附的个性化风险预测工具提供了在临床环境中实施该模型的实用方法,有可能改善骨科实践中的风险分层和患者护理。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

International Journal of Medical Informatics
医学-计算机:信息系统
CiteScore
8.90
自引率
4.10%
发文量
217
审稿时长
42 days
期刊介绍:
International Journal of Medical Informatics provides an international medium for dissemination of original results and interpretative reviews concerning the field of medical informatics. The Journal emphasizes the evaluation of systems in healthcare settings.
The scope of journal covers:
Information systems, including national or international registration systems, hospital information systems, departmental and/or physician''s office systems, document handling systems, electronic medical record systems, standardization, systems integration etc.;
Computer-aided medical decision support systems using heuristic, algorithmic and/or statistical methods as exemplified in decision theory, protocol development, artificial intelligence, etc.
Educational computer based programs pertaining to medical informatics or medicine in general;
Organizational, economic, social, clinical impact, ethical and cost-benefit aspects of IT applications in health care.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


