Kidney disease, diabetes, and diameter stenosis predict Rotablation bailout in modified balloon application for severely calcified coronary lesions
Abstract
Background
Modified balloon (MB) treatment in severely calcified coronary artery lesions is an established technique. However, some lesions require Rotablation (RA) as bailout strategy.
Aims
This study aimed to assess predictors of switch from MB to RA and its impact on procedural and midterm outcomes.
Methods
Four hundred and eighty-three consecutive patients were included undergoing MB treatment (n = 204) with a scoring or cutting balloon, or upfront RA treatment (n = 279) serving as control cohort. Strategy switch from MB to RA was performed in 19 of 204 patients. Procedural success was defined as successful stent implantation and TIMI III flow.
Results
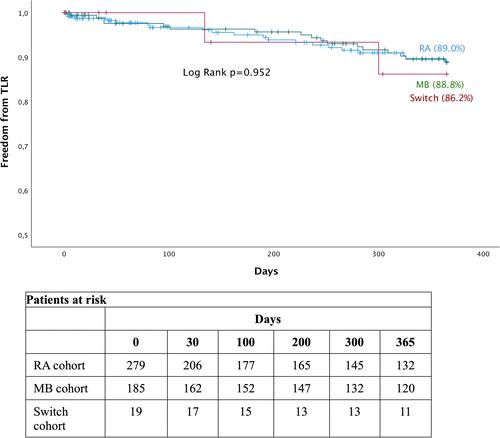
In the MB cohort, median age was 72 [63−78] years, 75.5% were male and 42.1% had acute coronary syndrome. Procedure success was achieved in 89.4% of the switch group versus 98.4% of the MB only group (p < 0.001) and in 96.4% of the RA cohort. In the switch group, periprocedural complications (31.6% vs. 8.1% vs. 11.8%, p = 0.007), radiation dose (149 [126–252] vs. 59 [30–97] vs. 102 [59–156] Gcm2; p < 0.001) and contrast volume (250 [190–250] vs. 190 [150–250] vs. 195 [190–-250] mL; p < 0.001) were significantly higher. Diabetes (OR 3.8, 95% CI 1.1–13.9, p = 0.042), chronic kidney disease stage 4 or 5 (OR 19.0, 95% CI 3.3–108.6, p < 0.001) and pronounced calcification resulting in higher angiographic diameter stenosis (OR 1.13, 95% CI 1.1–1.2, p = 0.001) independently predicted strategy switch. Midterm results were not affected by strategy switch regarding 1-year target lesion revascularization rates (86% vs. 89% vs. 89%; log-rank p = 0.95).
Conclusion
Primary RA strategy might be considered in patients with severely calcified coronary artery lesions with high angiographic diameter stenosis, diabetes or impaired renal function due to increased periprocedural complication rates, radiation dose, and contrast volume following strategy switch.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


